All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The pso Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the pso Hub cannot guarantee the accuracy of translated content. The pso and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The PsOPsA Hub is an independent medical education platform, supported by educational grants. We would like to express our gratitude to the following companies for their support: UCB, for website development, launch, and ongoing maintenance; UCB, for educational content and news updates. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View psoriasis and psoriatic arthritis content recommended for you
Psoriasis: An overview
Do you know... What approximate percentage of individuals with psoriasis will develop psoriatic arthritis in their lifetime?
Psoriasis is a chronic inflammatory condition that affects approximately 2–3% of the global population.1 Psoriasis can occur alongside other conditions, including cardiovascular disease, Crohn’s disease, and psoriatic arthritis.1 Plaque psoriasis is the most common type, accounting for approximately 80–90% of cases.2,3 Other types of psoriasis include guttate, pustular, inverse, and erythrodermic psoriasis.2,3
Psoriasis can have a significant impact on quality of life and is associated with metabolic, cardiovascular, and psychological comorbidities.2,3 In recent years, there have been advances in the understanding of the pathogenesis and genetics of psoriasis, and there have been multiple new biologics approved.
Here, we provide a summary of the etiology, epidemiology, pathophysiology, clinical manifestations, diagnostic tests and tools, and treatment options available for psoriasis.
Etiology2
Psoriasis can be caused by genetic and environmental triggers. Multiple identified alleles have been linked to psoriasis, including HLA-Cw6 and HLADQ*02:01, and loci, including PSORS1–9 and PSORSASI. Around 40% of people will develop psoriasis if both parents are affected. In genetically susceptible individuals, onset of psoriasis can be exacerbated by environmental factors such as skin trauma, infections, medications (including lithium), stress, and smoking. Around one-third of psoriasis patients develop psoriatic arthritis during their lifetime. Moreover, there are several comorbidities associated with psoriasis. These include:
- cardiometabolic disease (e.g., diabetes and stroke);
- psychological illness (e.g., depression and anxiety); and
- inflammatory bowel disease (e.g., Crohn’s disease and ulcerative colitis).
Epidemiology4
Approximately 125 million people worldwide have psoriasis. Studies suggest that psoriasis may be most common in northern Europe and least common in eastern Asia. Global disability burden of the disease tends to increase with age, with the greatest disease burden in individuals aged 50–69 years (Figure 1).
Figure 1. Epidemiology of psoriasis*
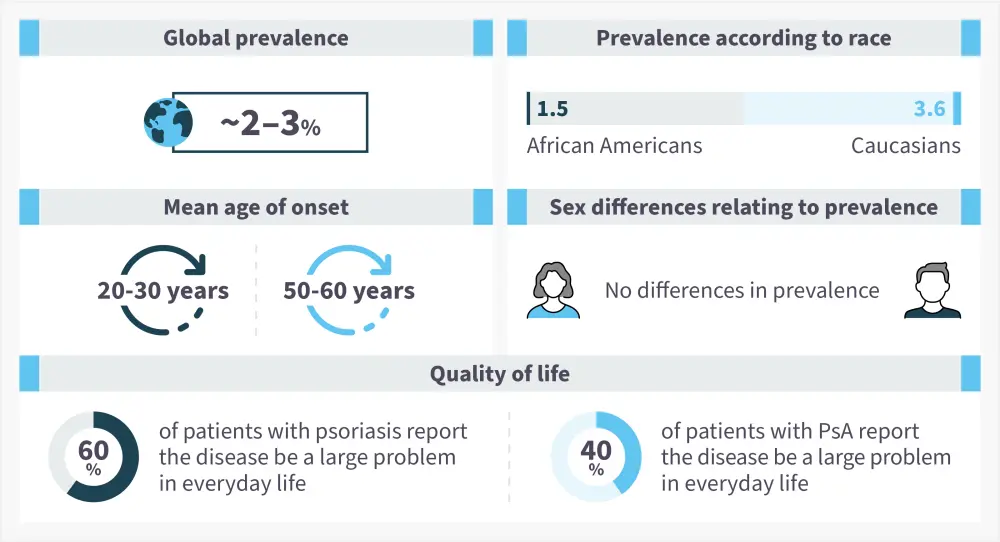
PsA, psoriatic arthritis.
*Data from National Psoriasis Foundation.4
Pathophysiology2
The pathophysiology of psoriasis is multifactorial and involves excessive activation of parts of the adaptive immune system, which can be partially due to environmental triggers (Figure 2).
Figure 2. Pathophysiology of psoriasis*
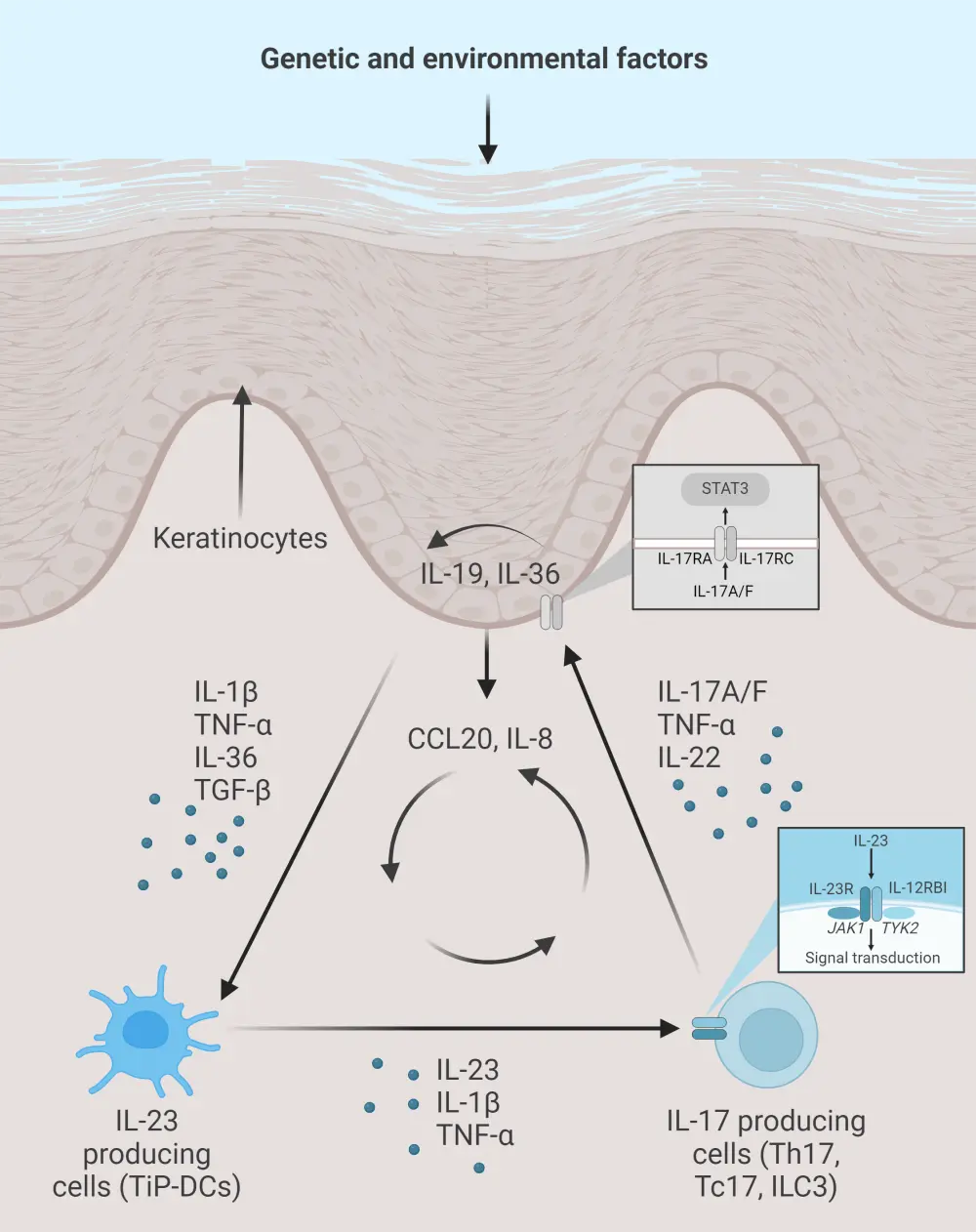
CCL, chemokine ligand; IL, interleukin; ILC, innate lymphoid cell; JAK, Janus kinase; STAT, signal transducers and activators of transcription; TGF, transforming growth factor; Th, T helper; TNF, tumor necrosis factor; TiP-DC, TNF and inducible nitric oxide synthase producing dendritic cell.
*Adapted from Armstong and Read.2 Created with BioRender.com
In the initial stages of psoriasis development, multiple cells including keratinocytes will secrete cytokines which activate myeloid dendritic cells. These cells secrete interleukins, inducing differentiation of naïve T cells to T helper cells. The T helper cells secrete interleukins and tumor necrosis factor alpha, leading to transcription of key inflammatory mediators and keratinocyte proliferation. This results in immune cell infiltration of the skin.
Signs and symptoms
There are multiple types of psoriasis.2 The most common type of psoriasis is plaque psoriasis (also called psoriasis vulgaris).2 Other types of psoriasis are inverse psoriasis, guttate psoriasis, erythrodermic psoriasis, pustular psoriasis, nail psoriasis, and scalp psoriasis.2,5 Signs and symptoms may differ across the types of psoriasis (Figure 3).5,6 Patients can have multiple types of psoriasis at the same time.5
Figure 3. Signs and symptoms of psoriasis*
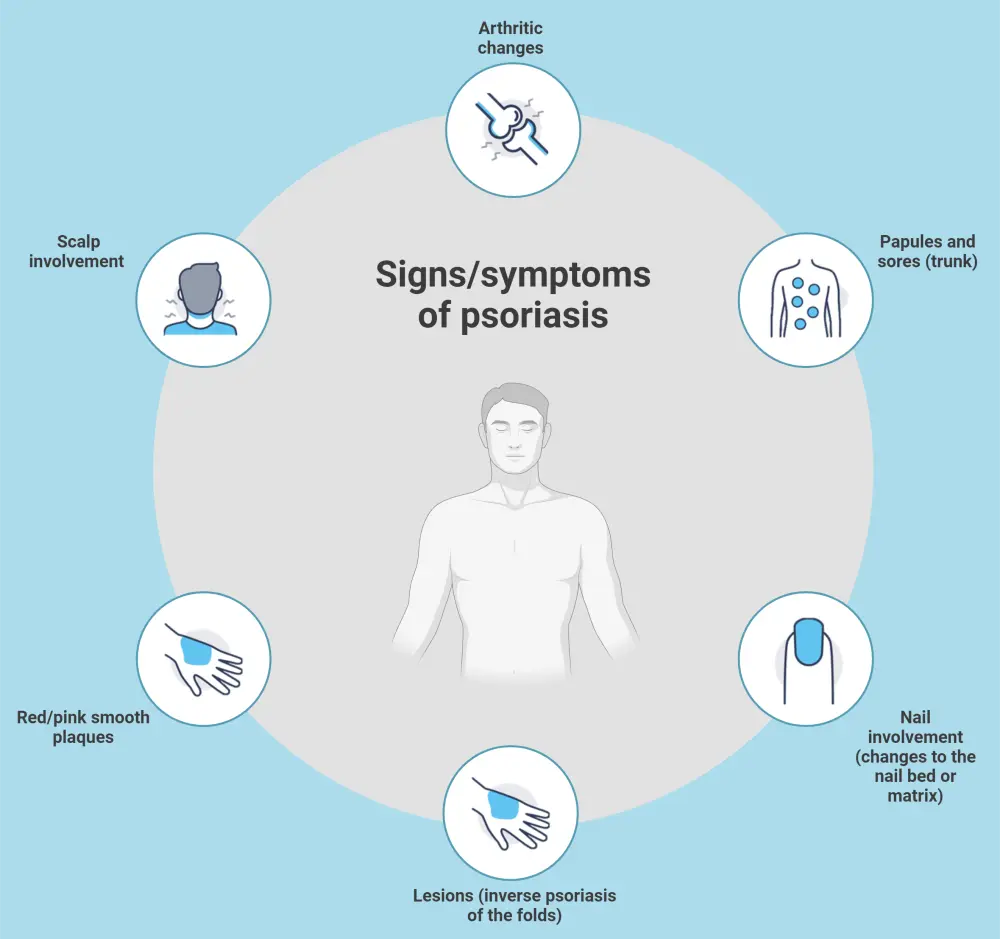
*Data from Gisondi, et al.6 Created with BioRender.com
Diagnosis
Due to the nature of psoriasis, it can be mistaken for other skin diseases, such as atopic dermatitis, seborrheic dermatitis, and pityriasis rosea.6 Diagnosis of psoriasis includes determining if there is a family history of psoriatic disease, and carrying out skin and nail examinations including morphology.6 The skin examination should be detailed, including the nails, scalp, flexures, and intergluteal cleft, as well as genital areas as patients may be embarrassed to discuss genital involvement.7 Psoriasis can often be diagnosed clinically, but skin biopsies may be required in atypical cases.6 Guidance on diagnosis may vary between countries; see the key guidelines section.
Management
Treatment strategies for psoriasis are based on psoriasis severity, presence of comorbidities, and patient preference and satisfaction.3 Some countries have adopted the concurrent use of biologics, oral agents, and phototherapies for moderate-to-severe plaque psoriasis.3 There is an increase in the treat-to-target approach, which may lead to better control of psoriasis and improved patient outcomes.8
There are many approved treatment options available for psoriasis. An overview of some of the available treatments is provided below (Figure 4).3
Figure 4. Overview of treatments available for psoriasis*
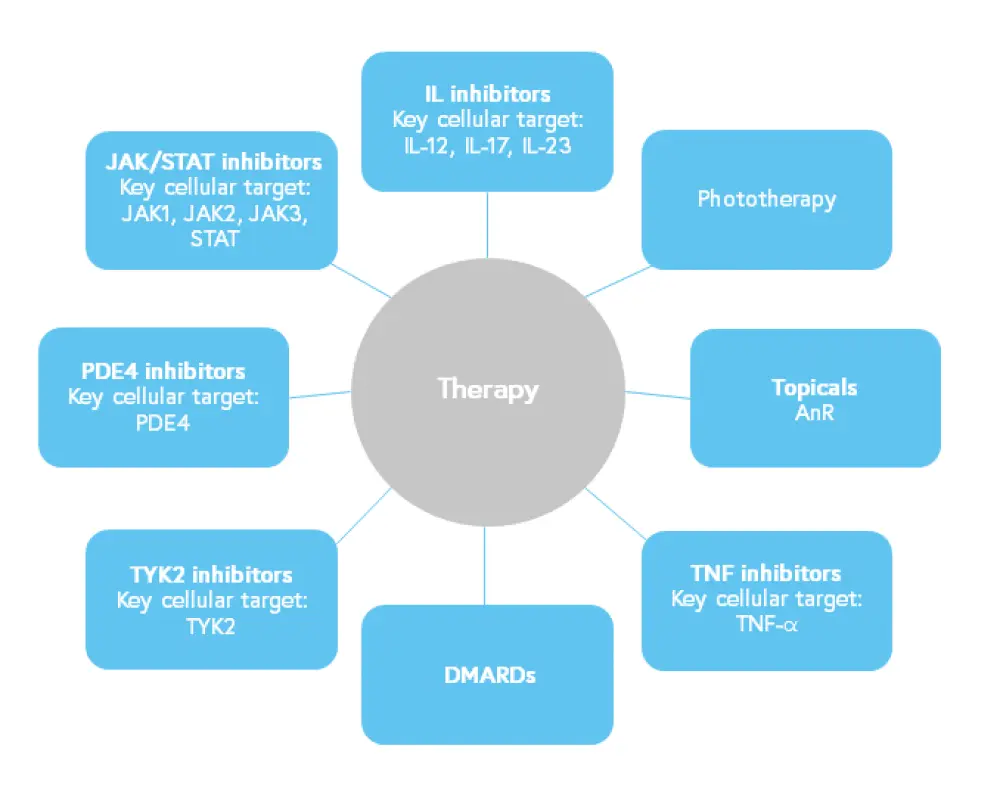
DMARD, disease-modifying antirheumatic drug; IL, interleukin; JAK, Janus kinase; PDE4, phosphodiesterase-4; STAT, signal transducers and activators of transcription; TNF, tumor necrosis factor; TYK2, tyrosine kinase 2.
*Data from Abdallah, et al.3
- A key drug approval timeline for psoriasis can be found here. Guidance on management may vary between countries; see below.
Key guidelines and organizations
EU guidelines
- EuroGuiDerm Guideline on the systemic treatment of psoriasis vulgaris
- EuroGuiDerm Guideline on the systemic treatment of psoriasis vulgaris–Part 2: specific clinical and comorbid situations
US guidelines
UK guidelines
Chinese guidelines
Medical societies/working groups
Patient organizations
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with plaque psoriasis do you see per month?

