All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The pso Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the pso Hub cannot guarantee the accuracy of translated content. The pso and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The PsOPsA Hub is an independent medical education platform, supported by educational grants. We would like to express our gratitude to the following companies for their support: UCB, for website development, launch, and ongoing maintenance; UCB, for educational content and news updates. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View psoriasis and psoriatic arthritis content recommended for you
The effect of sex differences on quality of life in patients with psoriatic arthritis
Clinical manifestations of psoriatic arthritis (PsA) can vary, with symptoms including joint pain, spinal pain, skin and nail psoriasis, and fatigue, which can all lead to reduced quality of life (QoL).1 Symptoms can differ between patients, with sex potentially playing a role in the manifestation of disease. Previous data suggest that women are more likely to have polyarticular disease and suffer greater disability than men, who are more commonly affected by axial disease.1
Here, we discuss a cross-sectional survey assessing the differences in disease burden in male and female patients with PsA. You can find additional information of the effect of sex on adverse drug reactions in our previous article.
Study design1
Data used in this study was collected from a survey (the Adelphi PsA Disease Specific Programme) of patients and their dermatologists/rheumatologists across France, Germany, Italy, Spain, United Kingdom, and United States in 2018. Patients were recruited when visiting their rheumatologist or dermatologist for routine care or diagnosis. The data collection design is shown in Figure 1.
Figure 1. Study design*
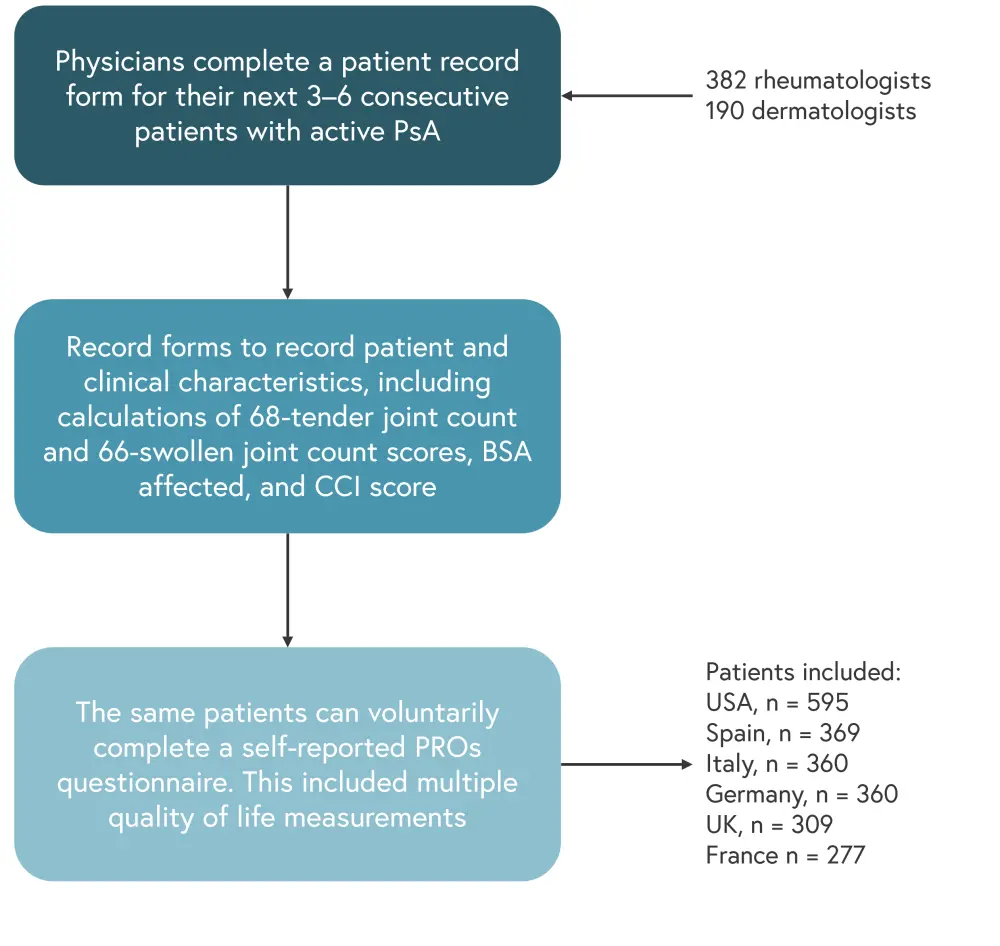
BSA, body surface area; CCI, Charlson Comorbidity Index; PROs, patient reported outcomes; PsA, psoriatic arthritis.
*Adapted from Gossec, et al.1
Results1
Physician-reported characteristics
Patient demographics and clinical characteristics were reported by the physician with a patient record form. The patient characteristics at the time of completing the record form are shown in Table 1. Both men and women had an average PsA duration of ~5 years, with a higher proportion of men being employed full-time compared to women. On average, women experienced fewer comorbidities than men.
Table 1. Patient characteristics*
|
BSA, body surface area; CCI, Charlson comorbidity index; PsA, psoriatic arthritis. |
|||
|
Characteristic, % |
Women |
Men |
p value |
|---|---|---|---|
|
Mean age, years |
48.3 |
48.8 |
0.42 |
|
Employment† |
|
< 0.01 |
|
|
Working full-time |
49.4 |
68.6 |
|
|
Working part-time |
8.6 |
5.1 |
|
|
On long-term sick |
1.4 |
3.5 |
|
|
Homemaker |
18.7 |
1.6 |
|
|
Student |
2.9 |
2.4 |
|
|
Unemployed |
5.8 |
4.7 |
|
|
Retired |
13.2 |
14.1 |
|
|
Mean CCI, score |
1.10 |
1.15 |
< 0.01 |
|
Mean PsA duration, years‡ |
4.87 |
4.95 |
0.42 |
|
Receiving biologic treatment |
53.7 |
55.1 |
0.38 |
|
Mean BSA involvement, score§ |
5.5 |
5.5 |
0.87 |
|
Mean 68-tender joint count, score‖ |
3.2 |
3.5 |
0.39 |
|
Mean 66-swollen joint count, score¶ |
4.1 |
4.5 |
0.03 |
The differences in tender and swollen joint counts are shown in Figure 2. Men had a higher mean swollen joint count compared to women (4.5 vs 4.1; p = 0.03); however, there was no statistical difference in tender joint count between men and women.
Figure 2. Tender joint count and swollen joint count*
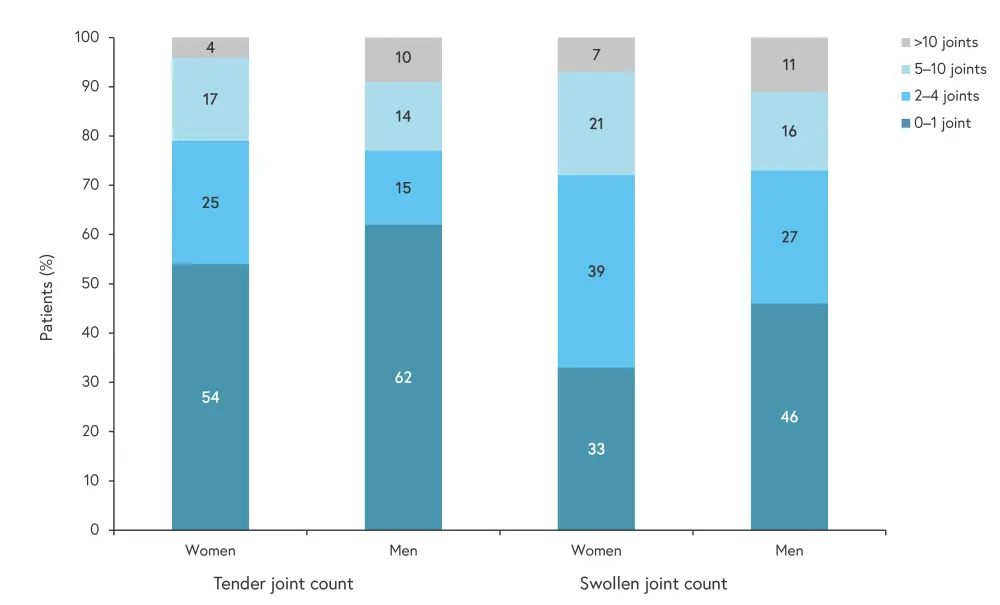
*Adapted from Gossec, et al.1
Patient-reported outcomes
In this study, women reported a worse QoL (0.80 vs 0.82; p = 0.02) and greater disability (0.56 vs 0.41; p < 0.01) than men, as defined by the EuroQoL 5-dimension questionnaire (EQ-5D) utility scores and health assessment questionnaire disability index (HAQ-DI) scores. More women had a low or medium EQ-5D utility score compared with men (14.7% and 46.7% vs 11.6% and 42.5%, respectively). HAQ-DI scores and EQ-5D utility scores are shown in Figure 3 and Figure 4, respectively.
Figure 3. HAQ-DI scores*
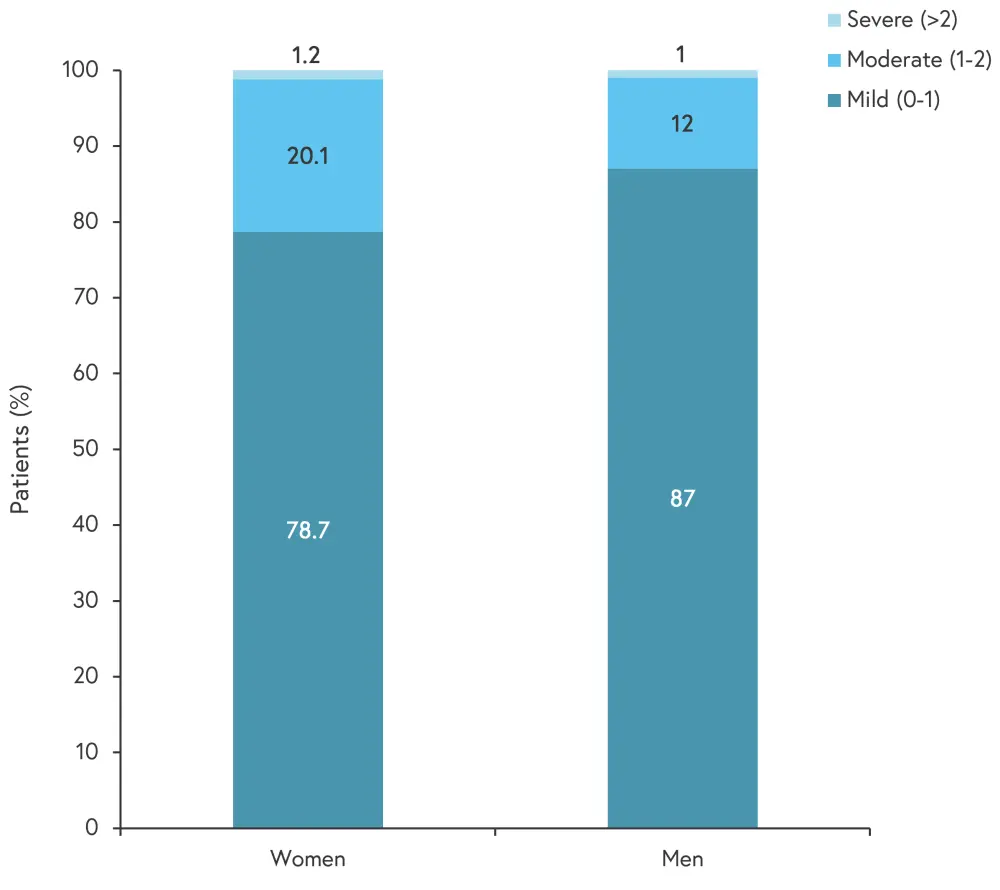
*Adapted from Gossec, et al.1
Figure 4. EQ-5D utility scores*
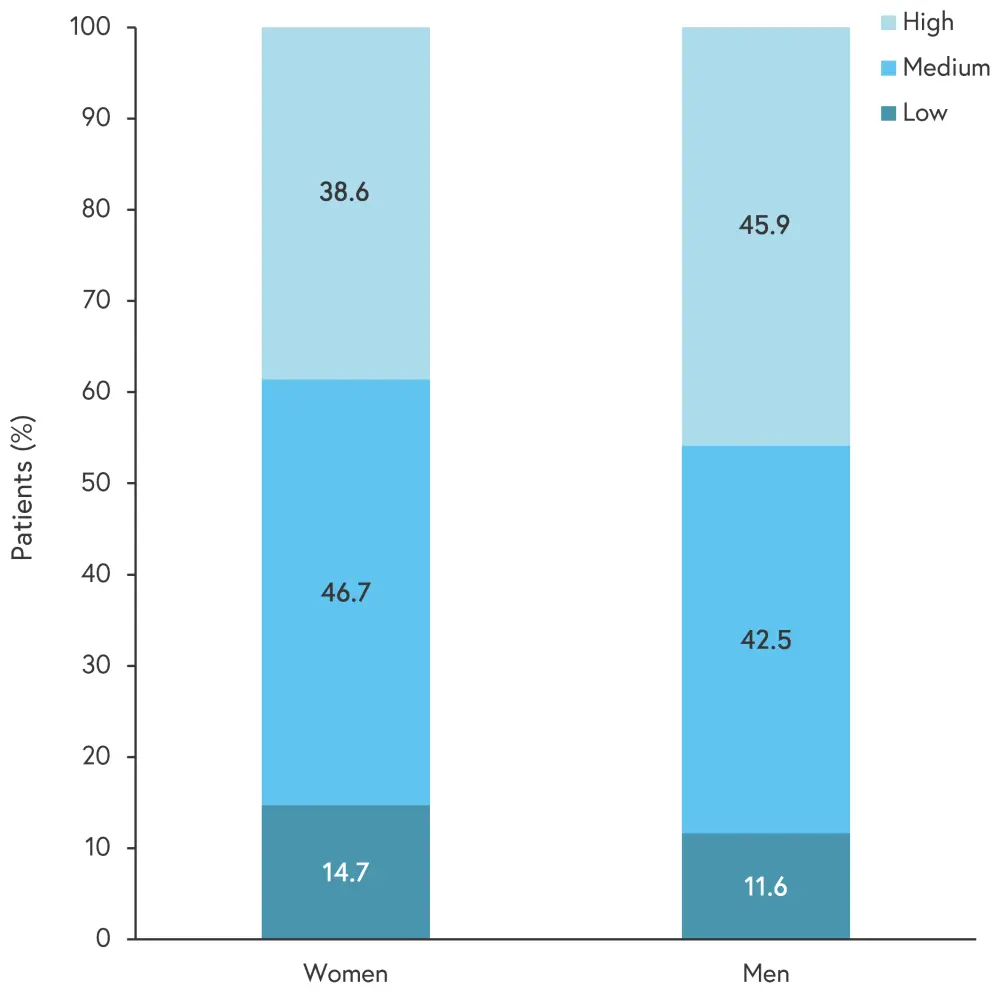
*Adapted from Gossec, et al.1
There was a greater proportion of women (22.4%) compared with men (16%) reporting an unacceptable 12-item PsA impact of disease (PsAID12) score, demonstrating that women were impacted to a greater extent by their psoriasis then men. In addition, women reported greater activity impairment compared with men (27.9% vs 24.6%; p < 0.01) as measured by the Work Productivity and Activity Impairment Questionnaire. However, this did not translate to greater work time missed for patients who were employed, there were no differences found for work time missed between men and women. Further details on work productivity and daily activity in patients with PsA can be found in one of our previous articles.
Conclusion1
Patients surveyed for this study had similar clinical characteristics, including disease activity and biologic use; however, women generally reported a worse QoL, with higher disability and work impairment compared to men, despite women experiencing fewer comorbidities. The authors noted several limitations of the study, including the self-reported nature of outcomes and the possible over-representation of patients who visit their physician more often.
Another study has suggested that women may experience higher disability, anxiety, and depression compared to men, with men achieving higher Psoriasis Area and Severity Index scores.2 Another factor contributing to observed sex-related QoL differences may be the use and efficacy of different treatments between men and women. An observational study found that among patients treated with a tumor necrosis factor inhibitor, women had worse patient-reported outcomes, with higher levels of anxiety and depression compared with men.3 The male patients on average were more likely to achieve a response after 6 months of treatment, with less side effects than women.3
Although it is not clear why these QoL differences occur, to the authors suggest that it may be due to the effect of sex hormones, differences in perceptions of pain, or differences in the way patients self-report disease impacts between sexes. Further research into these factors could provide insight into how treatment efficacy and QoL could be improved, with treatment regimens tailored to a patient’s sex.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with plaque psoriasis do you see per month?

