All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The pso Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the pso Hub cannot guarantee the accuracy of translated content. The pso and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The PsOPsA Hub is an independent medical education platform, supported by educational grants. We would like to express our gratitude to the following companies for their support: UCB, for website development, launch, and ongoing maintenance; UCB, for educational content and news updates. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View psoriasis and psoriatic arthritis content recommended for you
Special area involvement, disease severity, and treatments in a real-world psoriasis population
Diagnosis of psoriasis is often based on clinical features, rather than histological examination. The use of tools such as body surface area (BSA), Physician’s Global Assessment, and the Psoriasis Area and Severity Index can help clinicians categorize the severity of psoriasis. However, these tools do not account for disease impact in special areas, such as the face, scalp, and genitals.
Here, we summarize a study by Horner et al.1 in Dermatology and Therapy, which described BSA distribution, special area involvement, and available treatments, to evaluate disease burden in a real-world setting.
Study design and patient population1
- This retrospective study evaluated 5,120 patients with a BSA measured between 2014–2020.
- Patients were aged ≥18 years, with at least one diagnosis of psoriasis within 90 days before and after the index date (the date of the first BSA value identified for the patient in the included data).
- BSA categories at baseline:
-
- 23.4% of patients had a BSA of <3%
- 41.9% of patients had a BSA of 3–10%
- 34.6% of patients had a BSA of >10%
- Around half (49.3%) of patients were female, the majority were White (83.2%), and the most common comorbidities at baseline were hypertension (21.9%) and hyperlipidemia (17.8%).
Key findings1
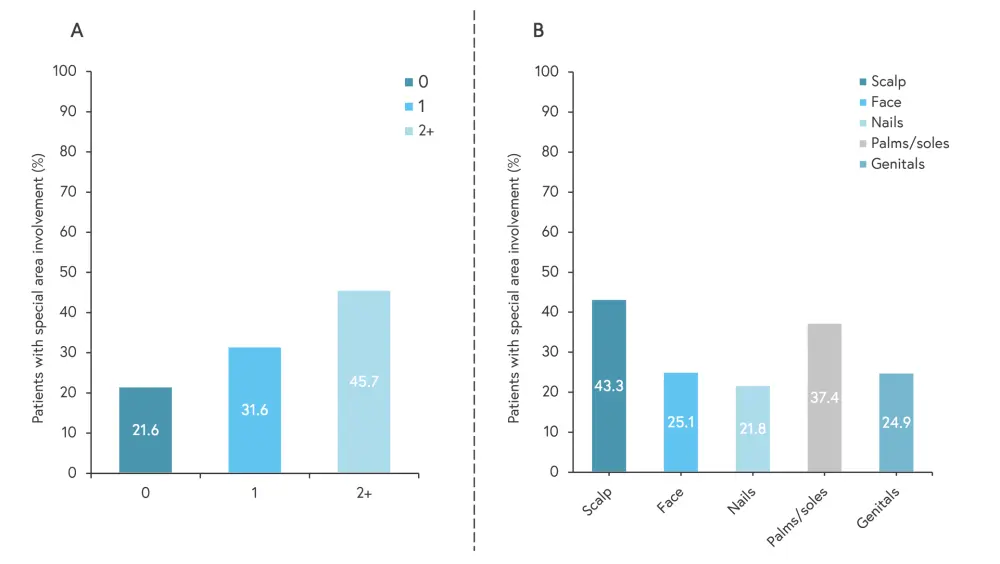
- In this real-world population, 77.3% had involvement in at least one special area (Figure 1A).
- Areas of involvement are shown in Figure 1B, the most common special area involved was the scalp (43.3%).
- The proportion of patients with involvement in two or more special areas was similar across the BSA categories.
- Of the 4,470 patients evaluated for initial treatment, majority received biologics (31.1%) or topicals (41.5%) only. 78.9% of patients received any topicals alongside other treatments.
- In patients with involvement of two or more special areas, the most common initial treatment was conventional synthetic anti-rheumatic drugs (54.1%), followed by topicals (48.3%), biologics (43.8%), and apremilast (43.5%).
Figure 1. A Several special areas are involved, and B prevalence of special areas by body location*
*Adapted from Horner, et al.1
|
Key learnings |
|
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with psoriatic arthritis do you see per month?


