All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The pso Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the pso Hub cannot guarantee the accuracy of translated content. The pso and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The PsOPsA Hub is an independent medical education platform, supported by educational grants. We would like to express our gratitude to the following companies for their support: UCB, for website development, launch, and ongoing maintenance; UCB, for educational content and news updates. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View psoriasis and psoriatic arthritis content recommended for you
The effect of sex differences in patient perception of PsA
Studies have suggested that PsA treatment satisfaction can vary between patients and their physicians, which can negatively impact quality of life; however, this may differ between patients of different sexes. Although the incidence of PsA is similar between male and female patients, observational studies have shown that females report greater loss of function and are more likely to experience pain.1,2
Here, we report results from a post-hoc analysis assessing the impact of sex differences in patients with PsA, presented by Eder at the European Alliance of Associations for Rheumatology (EULAR) 2023 Congress.1
Survey design1
Eligible patients were aged ≥18 years and had a self-reported diagnosis of PsA for at least one year prior to participation, reported using at least one biologic or synthetic disease-modifying anti-rheumatic drug, and visited a rheumatologist or dermatologist in the past 12 months. The survey design is shown in Figure 1.
Figure 1. Survey design*
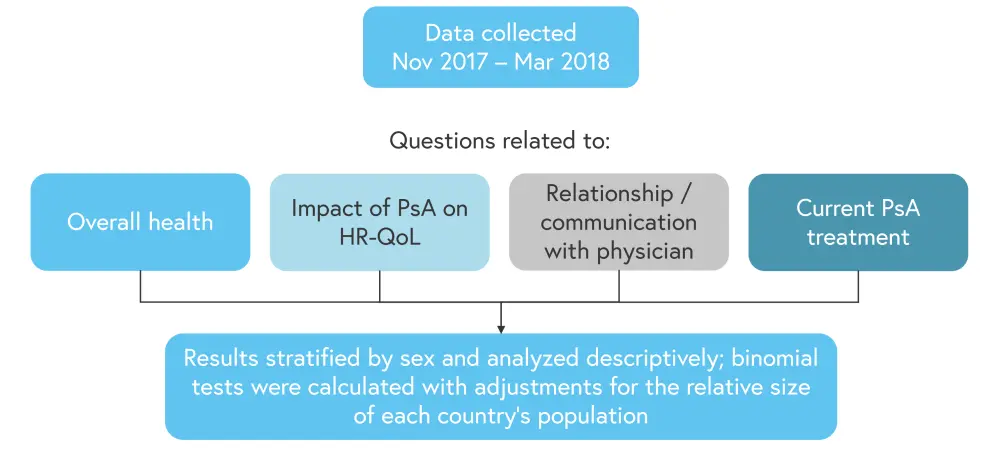
*Data from Eder.1
Results1
Overall, 1,286 patients with PsA both met the inclusion criteria and responded to the survey. Patient characteristics were similar between the sexes; however, more female patients had taken steroids for their PsA and more were currently taking a disease-modifying anti-rheumatic drug. In addition, female patients were more likely to have a diagnosis of anxiety or depression and were more likely to be affected by osteoarthritis. Patient characteristics are shown in Table 1.
Table 1. Selected patient characteristics*
|
DMARD, disease-modifying anti-rheumatic drug; NSAID, non-steroidal anti-inflammatory drug; PsA, psoriatic arthritis. *Adapted from Eder.1 |
||
|
Characteristic, % (unless otherwise stated) |
Female |
Male |
|---|---|---|
|
Weighted global total (n), % |
52 (674) |
48 (612) |
|
Mean age, years |
41.3 |
41.0 |
|
Mean time since PsA diagnosis, years |
9.2 |
8.8 |
|
Country |
|
|
|
Australia |
2 |
4 |
|
Brazil |
22 |
27 |
|
Canada |
5 |
5 |
|
France |
7 |
10 |
|
Spain |
5 |
8 |
|
Taiwan |
2 |
4 |
|
UK |
8 |
9 |
|
US |
47 |
33 |
|
PsA medications ever taken |
|
|
|
Biologic |
70 |
66 |
|
DMARD |
72 |
67 |
|
NSAID |
62 |
56 |
|
Steroid |
57 |
43 |
|
Other prescription |
12 |
8 |
|
Current PsA medication |
|
|
|
Biologic DMARD only |
36 |
39 |
|
Oral DMARD only |
32 |
33 |
|
Biologic and oral |
20 |
15 |
|
NSAIDs/steroids only |
10 |
12 |
Regarding the effect of PsA on quality of life, female and male patients reported a largely similar impact, with the exception of female patients reporting higher impact on their level of physical activity and their mental wellbeing compared with males (p < 0.05), as shown in Figure 2.
Figure 2. Quality of life impacts of PsA*
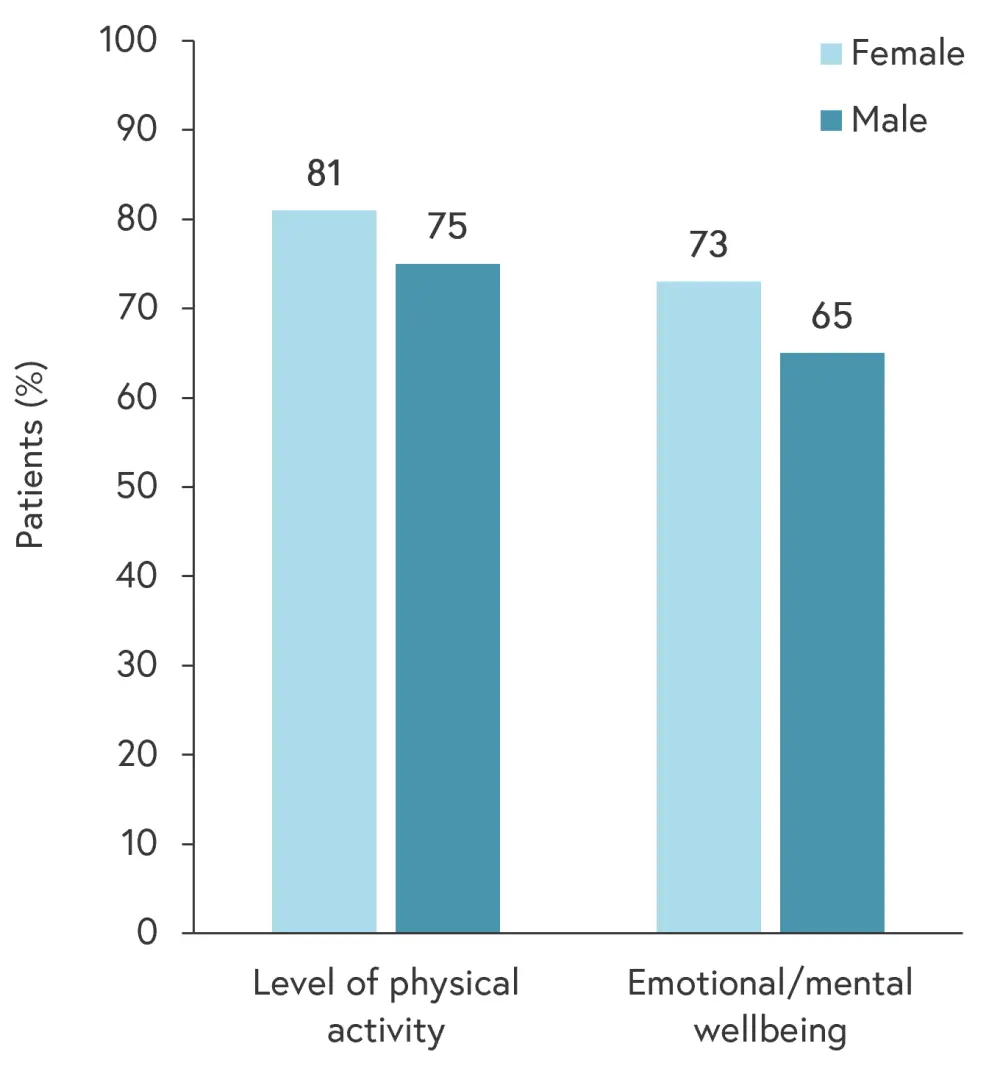
*Adapted from Eder.1
Female patients reported a greater social impact and were significantly more likely to go on permanent disability due to their PsA; however, men were more likely to experience decreased productivity at work, as shown in Figure 3.
Figure 3. Social and work impacts of PsA*
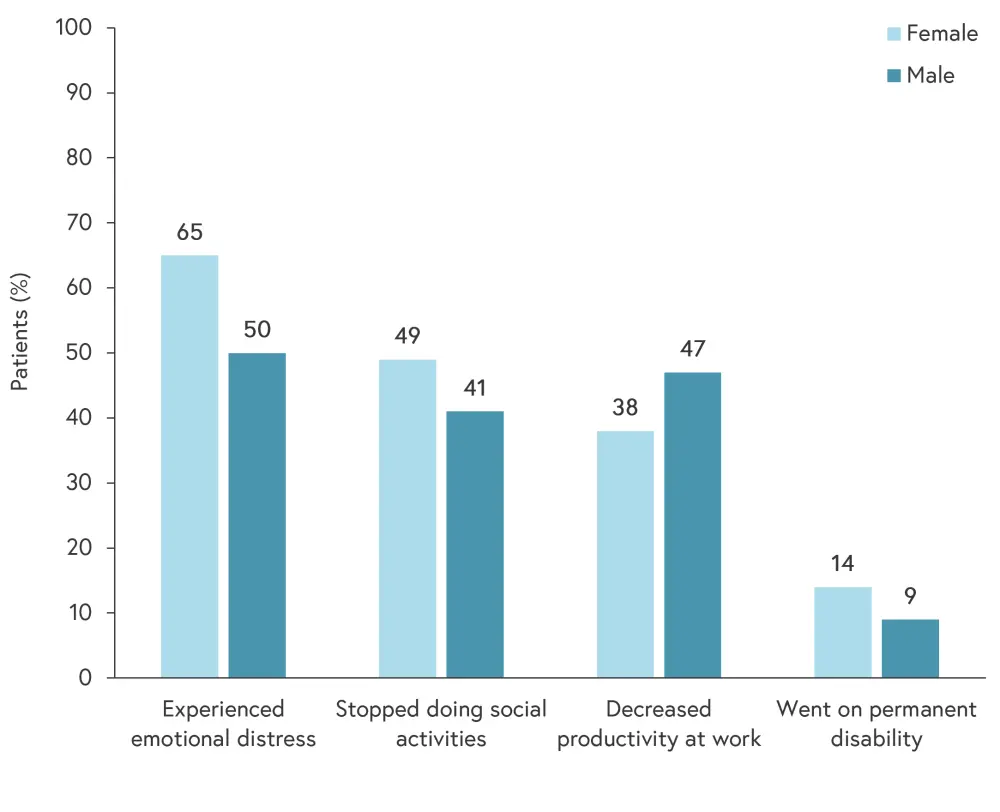
*Data from Eder.1
Female patients are more likely to discontinue treatment earlier. The most frequent reasons why patients switch or discontinue treatment are shown in Figure 4.1
Figure 4. Most frequent reasons for switching PsA treatment*
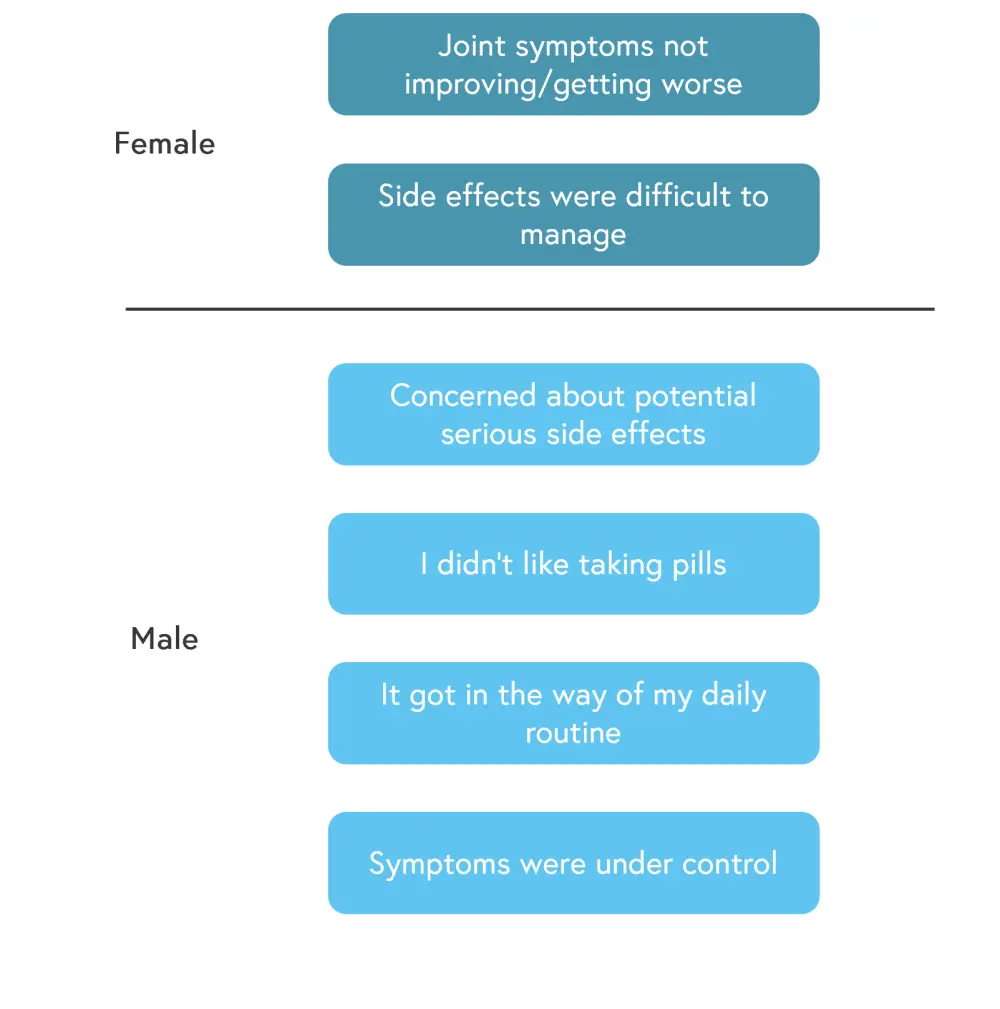
*Adapted from Eder.1
Finally, patient satisfaction with communication between them and their rheumatologist was assessed. A similar proportion of both male and female patients were somewhat or very dissatisfied with the communication, with the majority being very or somewhat satisfied. The proportions are shown in Figure 5.
Figure 5. Satisfaction with rheumatologist communication*
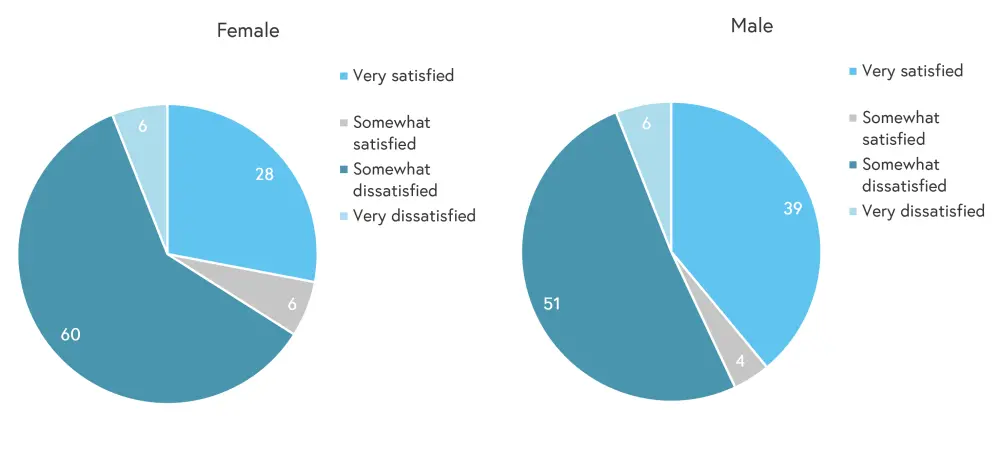
*Adapted from Eder.1
Conclusion
The speaker noted several limitations of this study, including the method of collection, as some patients may not have access to the internet; the majority of patients being from North America and Europe, as the results may not be representative of other regions; and the self-reported nature of the data.
However, this survey has demonstrated that female patients may experience a greater impact on their physical activity, mental wellbeing, and social life than male patients. Effects on work also differed between the sexes. Therefore, physicians should consider the impact of PsA on an individual basis and tailor support and treatment options accordingly.1
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with plaque psoriasis do you see per month?


