All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The pso Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the pso Hub cannot guarantee the accuracy of translated content. The pso and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The PsOPsA Hub is an independent medical education platform, supported by educational grants. We would like to express our gratitude to the following companies for their support: UCB, for website development, launch, and ongoing maintenance; UCB, for educational content and news updates. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View psoriasis and psoriatic arthritis content recommended for you
The association between cardiometabolic comorbidities and psoriasis in an ethnically diverse population: A cross-sectional analysis
Psoriasis has been linked to cardiometabolic comorbidities such as obesity, hypertension, and diabetes.1 However, many studies investigating this link primarily include White patients from wealthy backgrounds.1 Therefore, there is a lack of representation of ethnic minorities and poorer socioeconomic backgrounds.1
This cross-sectional analysis by Rudd et al.,1 published in Clinical and Experimental Dermatology compared the prevalence of cardiometabolic comorbidities in individuals with and without psoriasis in an ethnically and racially diverse, low-income population. The analysis aimed to assess whether ethnicity or race affects the risk of developing cardiometabolic comorbidities.1
Study design1
- Patients with and without psoriasis were identified between 2019–2022 from the San Francisco Health Network and were included if they had ≥2 primary care encounters and were aged ≥17 years during the study period.
- Clinical records were reviewed for demographics, smoking status, International Classification of Diseases 10th Revision codes, and clinical measurements.
- The primary outcome was the prevalence difference between patients with and without psoriasis for hypertension, hyperlipidemia, diabetes, and obesity (body mass index).
Key findings1
- A total of 56,987 patients were included, of which 926 had psoriasis. Of the patients with psoriasis, 61% were male and had a mean age of 59 years, compared with 55 years for patients without psoriasis (p < 0.001). The population had a high baseline prevalence of cardiometabolic comorbidities.
- Psoriasis was significantly associated with all the cardiometabolic comorbidities assessed in this study (Figure 1). The increased prevalence of these comorbidities in patients with psoriasis was similar across all racial and ethnic groups.
- Prevalence differences (adjusted for age and sex) for cardiometabolic comorbidities in patients with vs without psoriasis (all ethnicities and races combined) were:
- 5% for hypertension;
- 6% for hyperlipidemia;
- 3% for diabetes; and
- 10% for obesity.
- Although psoriasis appeared to be independently associated with cardiometabolic comorbidities, there was no evidence of effect modification based on race and ethnicity for the association of psoriasis with comorbidities.
Figure 1. Prevalence of hypertension†, hyperlipidemia‡, diabetes§, and obesity‖ in patients with and without psoriasis*
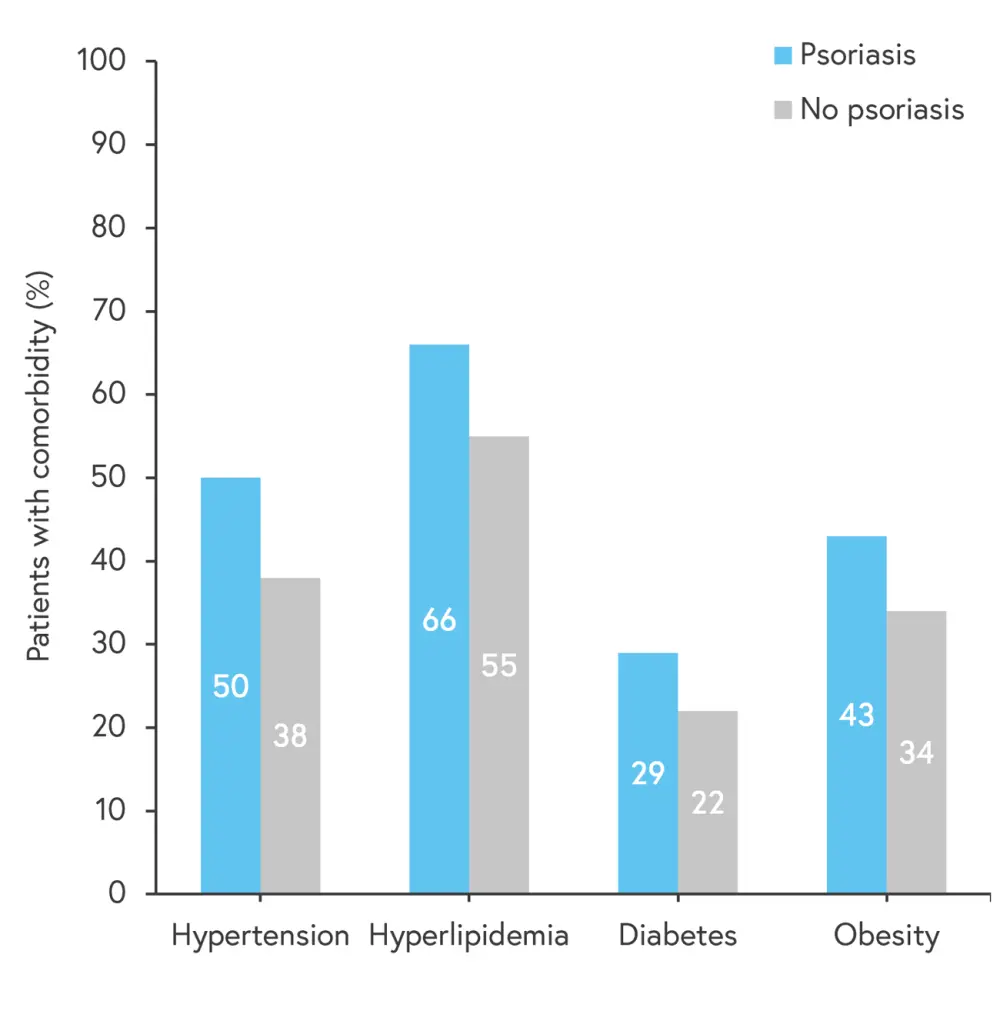
*Data from Rudd, et al.1
†Defined by the presence of the International Classification of Diseases 10th Revision (ICD-10) code.
‡Hyperlipidaemia was defined by the presence of ICD-10 code, or by total cholesterol ≥240 mg dL−1, triglycerides ≥150 mg dL−1, high-density lipoprotein <50 mg dL−1 for women and <40 mg dL−1 for men and low-density lipoprotein ≥160 mg dL−1.
§Diabetes was defined as the presence of an ICD-10 code, or hemoglobin A1c ≥6.5%.
‖Obesity was defined as BMI ≥30 kg m−2.
|
Key learnings |
|
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with plaque psoriasis do you see per month?


