All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The pso Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the pso Hub cannot guarantee the accuracy of translated content. The pso and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The PsOPsA Hub is an independent medical education platform, supported by educational grants. We would like to express our gratitude to the following companies for their support: UCB, for website development, launch, and ongoing maintenance; UCB, for educational content and news updates. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View psoriasis and psoriatic arthritis content recommended for you
Introduction
Ixekizumab (IXE), an interleukin (IL)-17 inhibitor, is approved for use in patients with active psoriatic arthritis (PsA).1 The Psoriasis and Psoriatic Arthritis Hub have previously reported on the use of IXE in psoriasis and PsA. There is currently limited data on the use of IXE with concomitant conventional synthetic disease-modifying antirheumatic drugs (csDMARDs).
In the 24-week results of the SPIRIT-P1 (NCT01695239) and SPIRIT-P2 (NCT02349295) trials, IXE demonstrated efficacy when used as a monotherapy and in combination with methotrexate.1 Here, we discuss the long-term safety and efficacy results of IXE in patients with PsA up to 152 weeks.
Study design1
SPIRIT-P1 and SPIRIT-P2 were both multi-center, double-blind, randomized phase III trials. The study design of both trials is shown in Figure 1. Patients in SPIRIT-P1 received treatment for up to 152 weeks, while patients in SPIRIT-P2 received treatment for 24 weeks but were evaluated for long-term safety and efficacy up to 156 weeks. Some patients were also receiving methotrexate, or another cDMARD, while on IXE.
Figure 1. Study design*
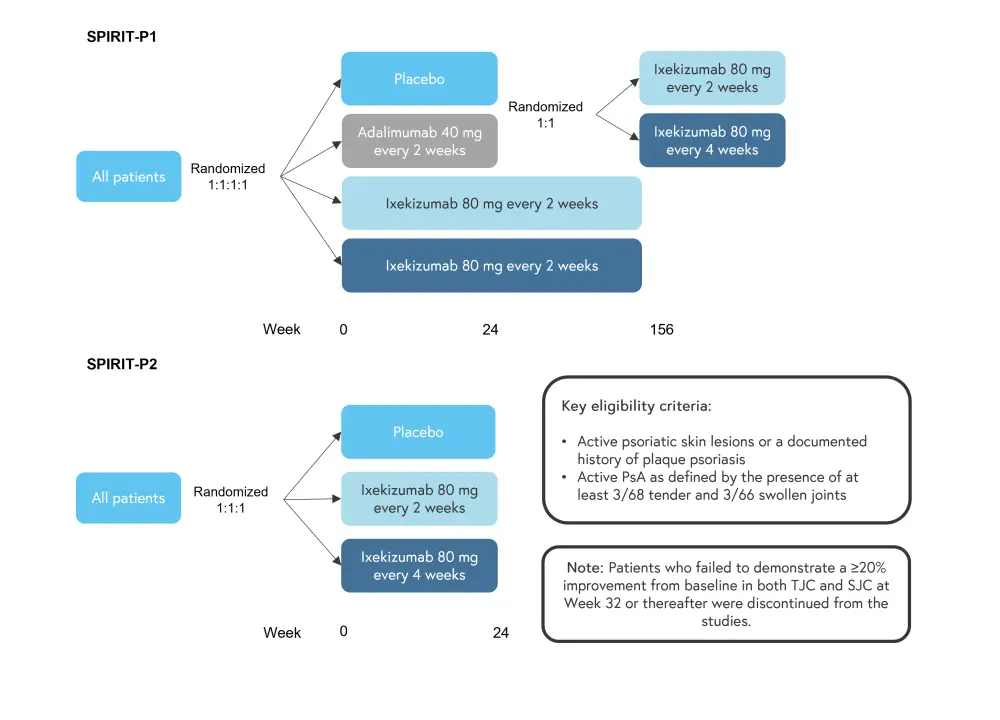
PsA, psoriatic arthritis; SJC, swollen joint count; TJC, tender joint count.
*Adapted from Coates, et al.1
Results1
Table 1. Baseline patient and disease characteristics*
|
BSA, body surface area; csDMARD, conventional synthetic disease-modifying antirheumatic drug; IXE, ixekizumab; LDI-B, Leeds Dactylitis Index-Basic; LEI, Leeds Enthesitis Index; MCS; mental component score; MTX, methotrexate; NAPSI, Nail Psoriasis Severity Index; PCS, physical component score; PASI, Psoriasis Area and Severity Index; SF-36, 36-Item Short Form Health Survey; TNFi, tumor necrosis factor inhibitor. |
|||
|
Characteristic, % (unless otherwise stated) |
IXE monotherapy |
IXE + MTX |
IXE + any csDMARD |
|---|---|---|---|
|
Mean age, years |
51.1 |
51.0 |
50.1 |
|
Male |
48.3 |
46.6 |
47.8 |
|
Race |
|
|
|
|
White |
96.6 |
90.9 |
91.2 |
|
Asian |
1.1 |
3.4 |
4.4 |
|
American Indian |
0 |
2.3 |
1.8 |
|
Native Hawaiian |
0 |
1.1 |
0.9 |
|
Black or African American |
1.1 |
0 |
0 |
|
Multiple |
1.1 |
2.3 |
1.8 |
|
Mean weight, kg |
87.8 |
87.4 |
87.3 |
|
Previous PsA systemic therapy |
|
|
|
|
No prior |
9 |
28.4 |
25.7 |
|
Non-biologic |
31.5 |
26.1 |
26.5 |
|
TNFi only |
0 |
23.9 |
21.2 |
|
TNFi and non- |
59.6 |
21.6 |
26.5 |
|
Corticosteroid use |
14.6 |
13.6 |
12.4 |
|
Mean time since PsA |
17.5 |
14.6 |
14.8 |
|
Disease characteristics |
|
|
|
|
Tender joints (68 |
22 |
20.7 |
21.0 |
|
Swollen joints |
12.2 |
11.6 |
12.3 |
|
LEI >0 |
55.1 |
61.4 |
59.3 |
|
LDI-B >0 |
27.6 |
29.9 |
31.8 |
|
PASI |
8.7 |
6.3 |
6.2 |
|
NAPSI† |
22.7 |
16.3 |
16.2 |
|
Affected BSA |
13.3 |
14.0 |
13.6 |
|
SF-36, score |
(n = 87) |
(n = 85) |
(n = 110) |
|
PCS |
32.5 |
32.6 |
32.7 |
|
MCS |
47.3 |
46.4 |
46.6 |
As shown in Table 1, the majority of patients were White, with a mean weight of ~87kg across the groups. In IXE monotherapy group, 50% more patients had previously received a tumor necrosis factor inhibitor and non-biologic compared with other groups.
Safety
Across SPIRIT-P1 and SPIRIT-P2, 229 patients were randomized to receive IXE 80 mg once every 4 weeks and analyzed to assess safety and efficacy. The majority of treatment-emergent adverse events (TEAEs) were mild or moderate, with a higher rate of discontinuation due to adverse events in patients only receiving IXE, compared to patients on IXE with methotrexate or any csDMARD. All groups had similar safety findings, although the patients treated with IXE monotherapy generally had a higher incidence of TEAEs (Figure 2).
Figure 2. TEAEs in patients randomized to IXE 80 mg once every 4 weeks*
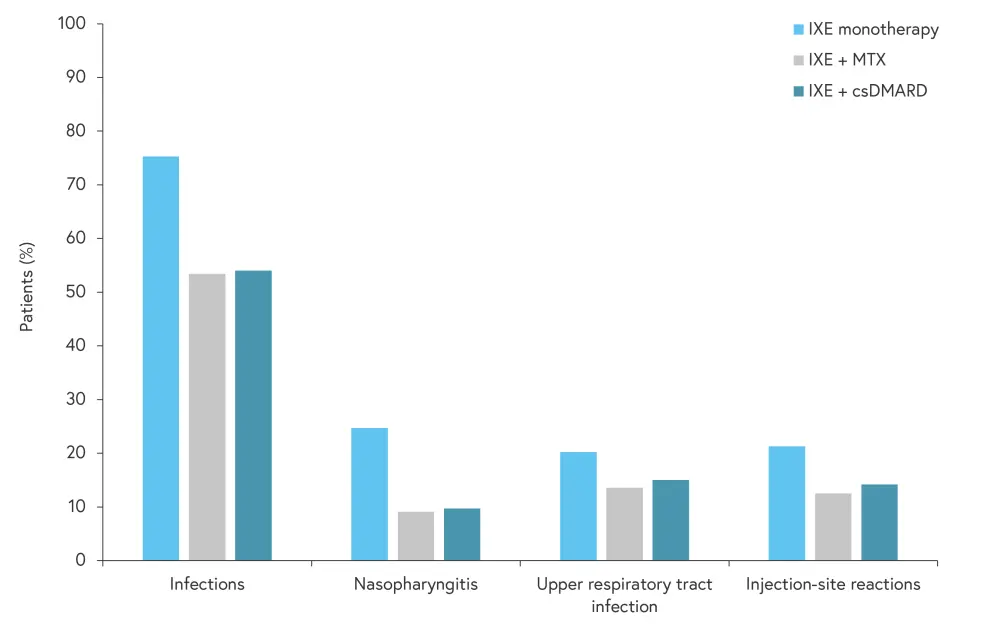
csDMARD, conventional synthetic disease-modifying antirheumatic drug; IXE, ixekizumab; MTX, methotrexate; TEAE, treatment-emergent adverse event.
*Adapted from Coates, et al.1
Efficacy
Improvements in PsA symptoms, defined by American College of Rheumatology (ACR) response, were seen in patients treated with IXE through to Week 156 in all groups (Figure 3). Around 60% of patients achieved ACR20 and ~30% of patients achieved ACR70 at Week 156. In addition, improvements were seen in psoriasis severity, with over 40% of patients in all groups achieving Psoriasis Area and Severity Index (PASI)100 at Week 156; PASI75, PASI90, and PASI100 scores at Week 156 are shown in Figure 4.
Figure 3. ACR20, ACR50, and ACR70 responses at week 156*
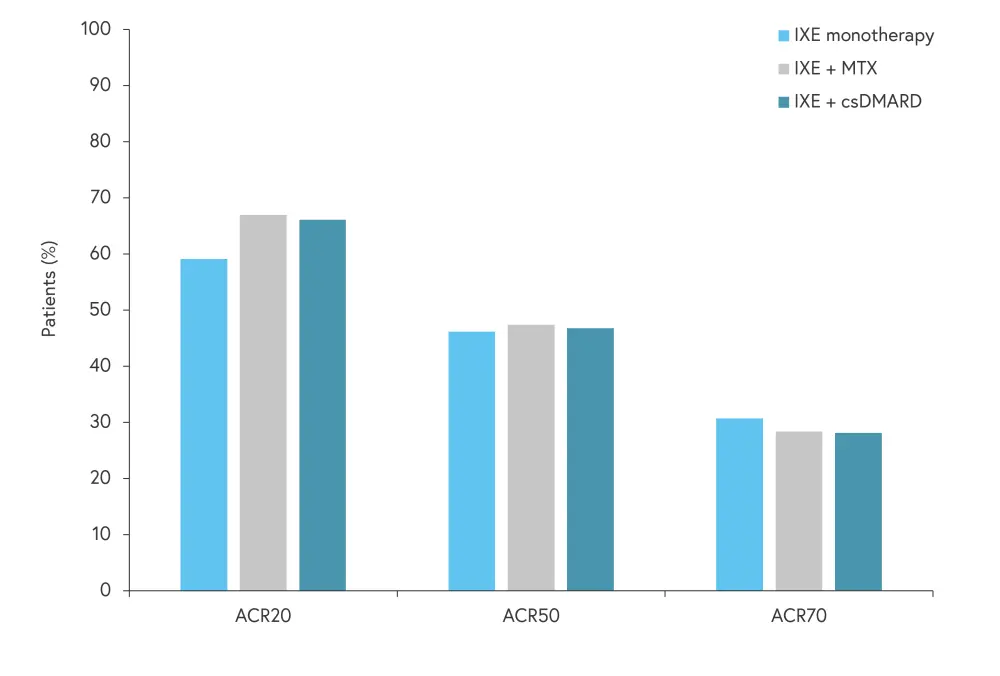
ACR, American College of Rheumatology; ACR20, ≥20% improvement in ACR response; ACR50, ≥50% improvement in ACR response; ACR70, ≥70% improvement in ACR response; cDMARD, conventional disease-modifying antirheumatic drug; IXE, ixekizumab; MTX, methotrexate.
*Adapted from Coates, et al.1
Figure 4. PASI75, PASI90, and PASI100 scores at week 156*
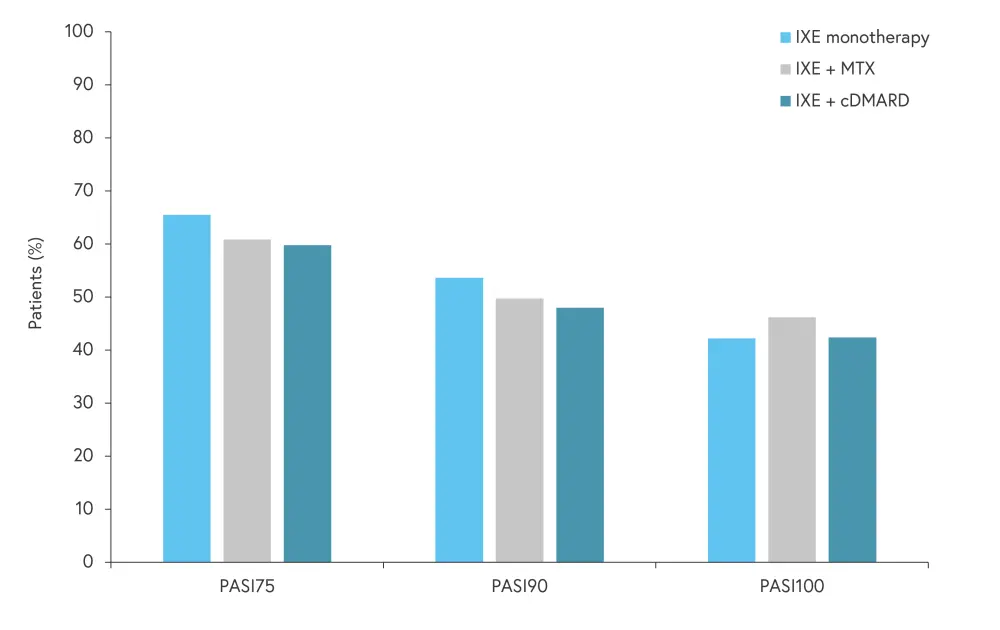
cDMARD, conventional disease modifying antirheumatic drug; IXE, ixekizumab; MTX, methotrexate; PASI, Psoriasis Area and Severity Index; PASI75, ≥75% reduction in PASI score from baseline; PASI90, ≥90% reduction in PASI score from baseline; PASI100, 100% reduction in PASI score from baseline.
*Adapted from Coates, et al.1
Conclusion
Results from SPIRIT‑P1 and SPIRIT‑P2 trials demonstrate the long-term safety and efficacy of IXE in patients with active PsA, both as monotherapy and in combination with csDMARDs such as methotrexate. The safety profile was consistent with previous data in this patient group; however, it is unclear if the higher incidence of adverse events in patients receiving IXE monotherapy is significant.1 The authors noted several limitations of this analysis, including a potential bias towards data from patients who remained in the study for the full 3 years and the relatively small subgroup sample sizes.1 Further trials, in larger cohorts, are warranted to confirm the safety and efficacy of IXE in patients with active PsA, both as monotherapy and in combination with csDMARDS.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with plaque psoriasis do you see per month?


 Laura Coates
Laura Coates