All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The pso Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the pso Hub cannot guarantee the accuracy of translated content. The pso and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The PsOPsA Hub is an independent medical education platform, supported by educational grants. We would like to express our gratitude to the following companies for their support: UCB, for website development, launch, and ongoing maintenance; UCB, for educational content and news updates. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View psoriasis and psoriatic arthritis content recommended for you
Ixekizumab: 5-year sustainability of scalp psoriasis clearance and patient-reported outcomes
Scalp involvement occurs in approximately 50-80% of individuals with psoriasis and can be difficult-to-treat with conventional non-systemic therapies.1 Scalp psoriasis affects patients socially and psychologically, and increases disease and itch severity compared with psoriasis in other body areas.1 Therefore, patient-reported outcomes are key in trials investigating scalp psoriasis.
Here, we summarize an analysis by Egeberg et al.1 published in Dermatology and Therapy on clinical and patient-reported outcomes after ixekizumab treatment in patients with scalp psoriasis over a 5-year period.1 Ixekizumab has not been studied specifically in scalp psoriasis, therefore this post hoc analysis focuses on a subset of patients with scalp psoriasis from the phase III UNCOVER-1, -2, and -3 trials.1
Study design1
-
UNCOVER-1 (NCT01474512), UNCOVER-2 (NCT01597245), and UNCOVER- 3 (NCT01646177) were double-blind, randomized phase III trials in patients with moderate-to-severe plaque psoriasis.
-
Psoriasis Scalp Severity Index (PSSI) was assessed from baseline through to 5 years.
-
Itch Numeric Rating Scale (NRS), Skin Pain Visual Analog Scale, and Dermatology Life Quality Index were used to assess patient-reported outcomes.
Key findings1
-
A total of 538 patients with scalp psoriasis who were treated with ixekizumab and had a PSSI measurement at Week 60 were included.
-
A high proportion of patients achieved a PSSI-0 (complete clearance of scalp psoriasis) at Week 60 (88.4% of patients from UNCOVER-1/2 and 75.9% of patients from UNCOVER-3).
-
Overall, ≥84.9% and ≥88.5% of patients maintained a PSSI-0 response at Week 60 through to Week 264 in UNCOVER-1/2 and UNCOVER-3, respectively.
-
In Week 60 PSSI-0 responders, substantial mean improvements from baseline to Week 12 were observed in all patient-reported outcome measures (Figure 1); these improvements were maintained to Week 264 (improvements of 94.3% in Dermatology Life Quality Index, 90.8% in Itch NRS, and 95.2% in Skin Pain Visual Analog Scale in UNCOVER-1/2).
Figure 1. Patient-reported outcomes at Week 12 and Week 256 in Week 60 PSSI-0 responders*
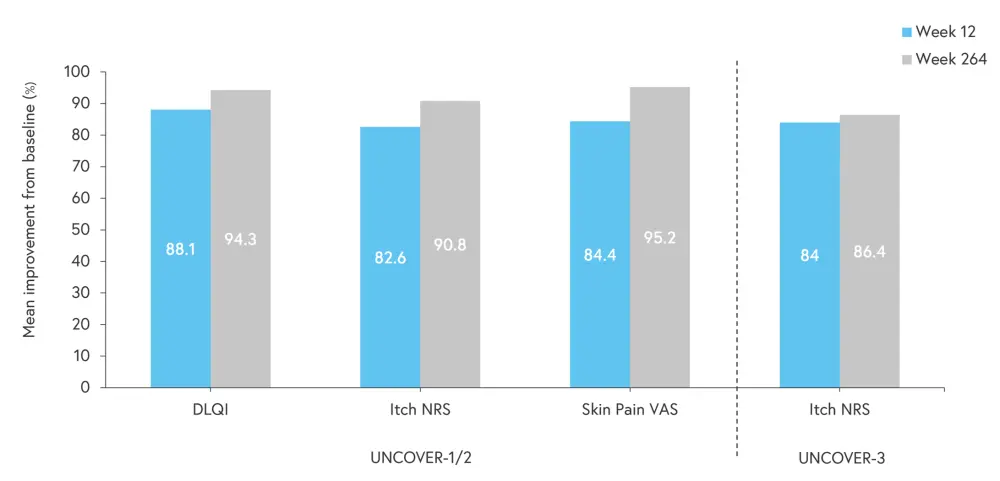
DLQI, Dermatology Life Quality Index; Itch NRS, Itch Numeric Rating Scale; PSSI, Psoriasis Scalp Severity Index; Skin Pain VAS, Skin Pain Visual Analog Scale.
*Data from Egeberg, et al.1
-
At Week 60, 70.7% and 73.2% of patients had concurrent PSSI-0 and a 100% improvement in Psoriasis Area and Severity Index in the UNCOVER-1/2 and UNCOVER-3 trials, respectively. This was maintained in the ranges of 70.7–61.3% and 73.2–58.5% to Week 264 in the UNCOVER-1/2 and UNCOVER-3 trials, respectively.
|
Key learnings |
|
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with plaque psoriasis do you see per month?

