All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The pso Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the pso Hub cannot guarantee the accuracy of translated content. The pso and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The PsOPsA Hub is an independent medical education platform, supported by educational grants. We would like to express our gratitude to the following companies for their support: UCB, for website development, launch, and ongoing maintenance; UCB, for educational content and news updates. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View psoriasis and psoriatic arthritis content recommended for you
Utilizing musculoskeletal ultrasound as a tool for early PsA detection
The transition state between psoriasis and psoriatic arthritis (PsA) can be difficult for patients, with PsA affecting their physical functioning and quality of life.1 Delays in the diagnosis of PsA, even by 6 months, can result in irreversible joint damage. Therefore, identifying individuals with psoriasis who are at risk of progression to PsA is key for earlier intervention.1
Here, we summarize a review by Ribeiro et al. published in Current Rheumatology Reports on the use of musculoskeletal ultrasound (MSUS) to detect subclinical inflammation, with the aim of identifying individuals who are at a higher risk of PsA development following psoriasis.1
MSUS in patients without musculoskeletal symptoms1
- Studies of ultrasound use in patients with psoriasis have found that patients frequently present with subclinical articular and entheseal abnormalities. This suggests that musculoskeletal inflammation occurs before clinical symptoms in some patients with PsA.
- In a study by Gisondi et al., psoriasis patients had higher Glasgow Ultrasound Enthesitis Scoring System (GUESS) compared with healthy controls (7.9 vs 2.9, p < 0.0001), with an increased mean tendon thickness.
- According to studies by Aydin et al. and Eder et al., bone erosion is almost always only observed in psoriatic disease (5–32% of patients with PsA, 2.9–6.1% of patients with psoriasis, and up to 0.4% of healthy controls).
MSUS as a tool for early PsA detection1
- A study by Grobelski et al., assessed the use of MSUS by trained dermatologists. MSUS scans performed by dermatologists were found to be comparable with those by rheumatologists in detection of joint effusion and synovial hyperperfusion.
- Preliminary data suggests that using MSUS measurements as part of the Classification for Psoriatic Arthritis (CASPAR) criteria could lead to increased accuracy and earlier PsA diagnosis.
- The European Alliance of Associations for Rheumatology (EULAR) and the Psoriasis and Psoriatic Arthritis Clinics Multicenter Advancement Network (PPACMAN) initiative have developed frameworks to identify subclinical PsA, which includes patients with arthralgia and/or positive MSUS findings. This makes it easier to initiate clinical trials to target patients at high risk of PsA development, who could benefit from preventative therapeutics.
Future perspectives1
- Extending MSUS to dermatologists, or even primary care physicians, could allow for earlier identification of PsA. A proposed treatment algorithm is shown in Figure 1, which can be used to both inform referral to rheumatology and to improve precision of the diagnosis, enabling timely intervention.
Figure 1. Suggested treatment algorithm for diagnosis of PsA incorporating MSUS*
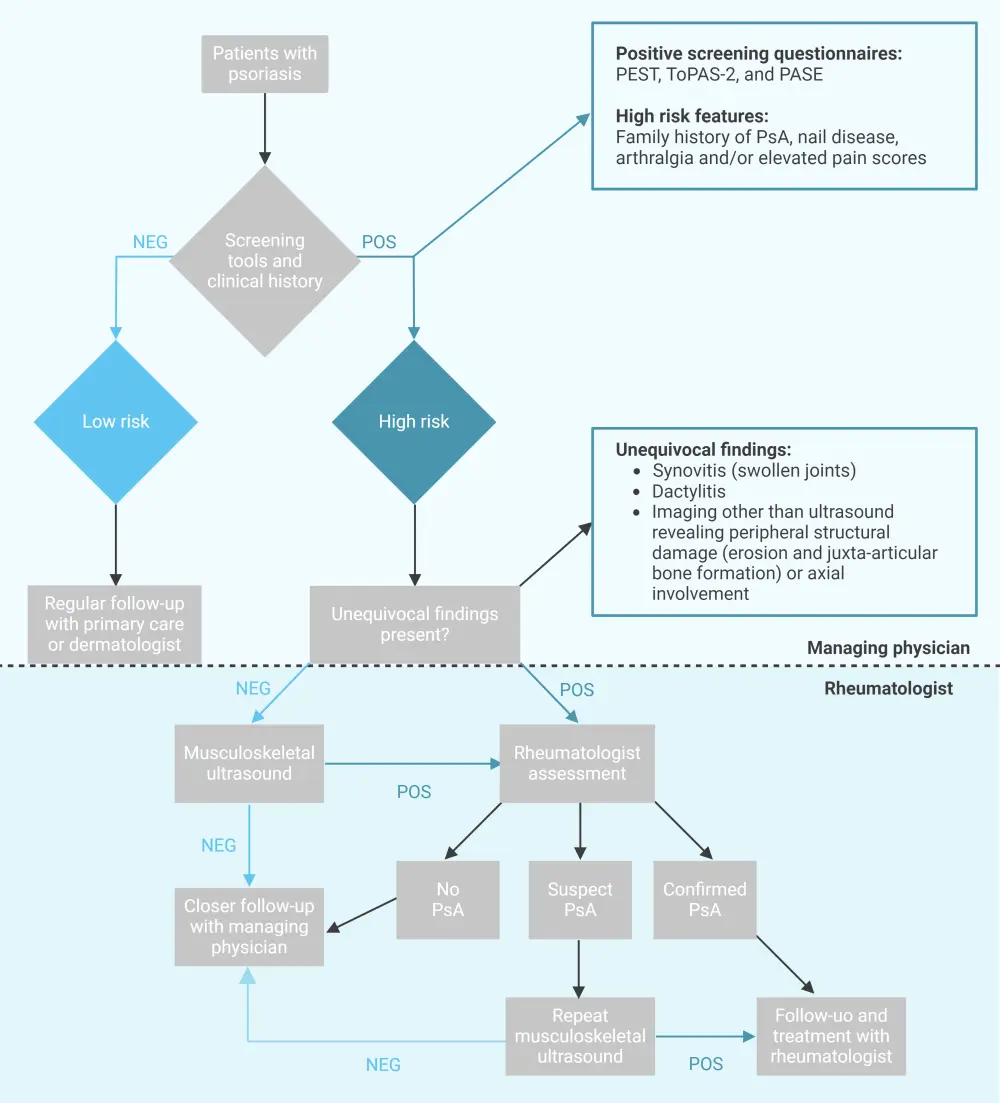
PsA, psoriatic arthritis; POS, positive; NEG, negative; PEST, Psoriasis Epidemiology Screening Tool; ToPAS-2, Toronto Psoriatic Arthritis Screen Version 2; PASE, Psoriatic Arthritis Screening and Evaluation.
*Adapted from Ribeiro, et al.1 Created with BioRender.com
|
Key learnings |
|
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with psoriatic arthritis do you see per month?

