All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The pso Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the pso Hub cannot guarantee the accuracy of translated content. The pso and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The PsOPsA Hub is an independent medical education platform, supported by educational grants. We would like to express our gratitude to the following companies for their support: UCB, for website development, launch, and ongoing maintenance; UCB, for educational content and news updates. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View psoriasis and psoriatic arthritis content recommended for you
Utilization of teledermatology in a post-COVID-19 era: Recommendations from the IPC
In recent years, technological advancements have enabled more effective communication between healthcare providers and their patients. The development of telemedicine (TM), whereby patients can contact their physician through videos and photos, has improved access to quality healthcare, especially for those in remote locations. However, TM is not yet well established and there is no consensus on the utility of TM in dermatology and rheumatology.
The International Psoriasis Council (IPC) have developed a TM working group to formulate a ‘call to action’ for the use of TM for patients with psoriasis. Here, we summarize statements made by the working group and discuss the future implications of TM in psoriasis treatment.
Members of the TM working group have clinical experience in treating psoriasis, competence in using TM, and exposure to teledermatology research. The group discussed various topics and provided statements on how TM could be optimized for patients with psoriasis. The main topics of discussion are shown in Figure 1.
Figure 1. Topics discussed by the IPC TM working group*
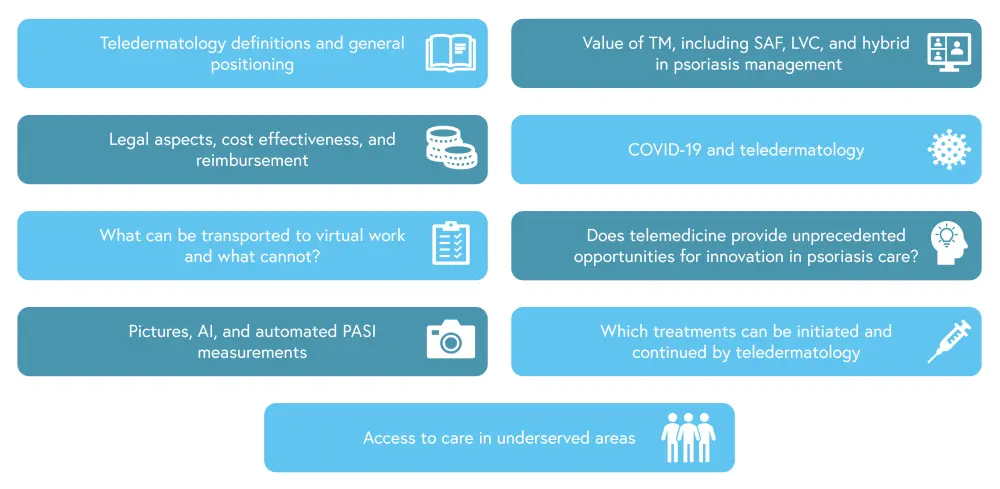
AI, artificial intelligence; LVC, live video conferencing; PASI, Psoriasis Area and Severity Index; SAF, store and forward; TM, telemedicine.
*Adapted from El Komy, et al.1
Discussion outcomes
Teledermatology definitions
TM uses electronic communication to deliver medical care to patients, without the need for face-to-face contact. Teledermatology relies on the communication of symptoms via photographs and videos, which is made possible by the visual nature of many dermatological conditions.
Teledermatology facilitates accessible care, which is especially important for economically disadvantaged patients or those facing lengthy waits to see a specialist. The IPC have committed to educating dermatologists about the potential of teledermatology.
The value of TM
Limitations of TM include the loss of physical contact, which may impact the doctor patient relationship; for patients with psoriasis, in-person care is still regarded as optimal. Also, patients may have concerns relating to doctor-patient confidentiality and, in some countries, patients may refuse TM based on cultural or religious differences with the physician.
Teledermatology can involve sending photos to a physician to be reviewed at a later date, using live video, telephone calls, or a hybrid approach. All these methods have benefits and limitations; therefore, the method of TM should be considered on a case-by-case basis. The IPC will provide a forum for healthcare professionals to discuss providing personalized care for patients with psoriasis, utilizing both TM and in-person consultations.
Legality and cost-effectiveness of TM
The German guidelines for teledermatology best practice provide guidance on implementation, patient information, and quality assurance. However, most countries do not have guidelines for the integration and reimbursement of TM services, despite the increased use of TM during the COVID-19 pandemic.
Previous studies have suggested that teledermatology is more cost-effective than in-person care, especially when indirect costs such as lost leisure time, loss of productivity, and costs to those accompanying the patient are taken into account. If reimbursement policies are altered, using TM could also allow for earlier diagnosis and initiation of therapy; however, this depends on whether reimbursement is covered by insurance or a national healthcare system. The IPC agreed to raise awareness of data protection, IT security, and the need to establish a reimbursement system for TM services.
Teledermatology during COVID-19
In a survey carried out during the COVID-19 pandemic, dermatologists reported delays in patient care. This impacted drug compliance, caused psychological distress, and worsened symptoms. Patient perceptions of TM, from a survey of 168 patients who attended telehealth appointments during the COVID‐19 pandemic under the George Washington Medical Faculty Associates Dermatology Department, are shown in Figure 2.
Figure 2. Patient perceptions of TM*
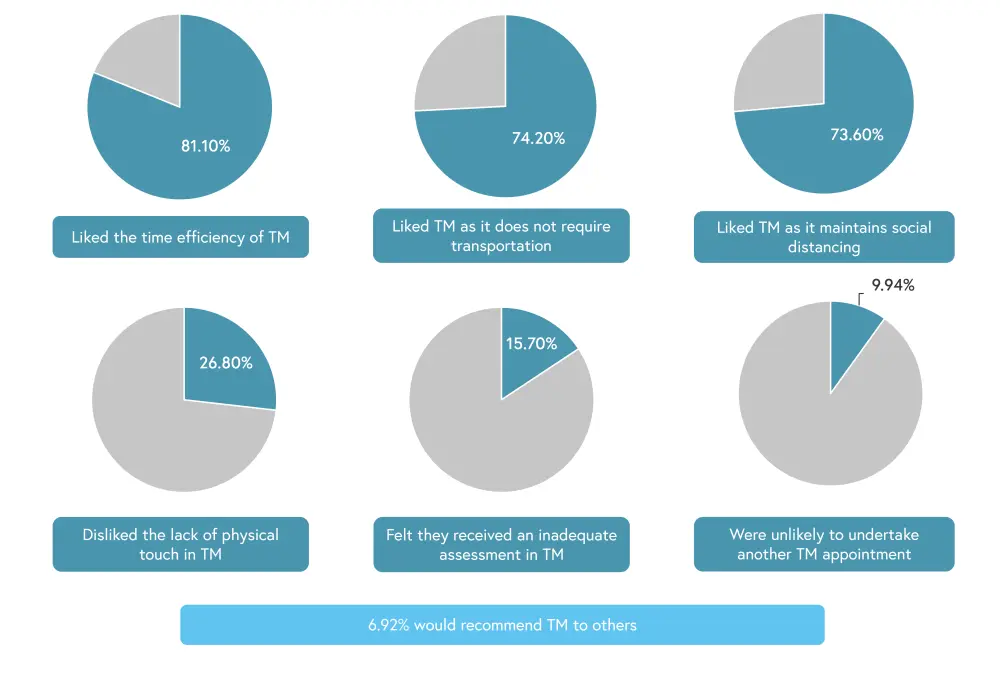
TM, telemedicine.
*Adapted from El Komy, et al.1 and Yeroushalmi, et al.2
In an Italian survey of patients with psoriasis, 48% of patients treated with biologics preferred TM over in-person care; however, elderly patients preferred in-person treatment. The IPC has a COVID-19 resource center, which shares information on how to use TM during lockdowns.
What can be transported to TM?
In a 12-week randomized trial, patients were assigned to receive either TM or in-person care for psoriasis. The results revealed that daily TM and educational tools allowed for improved Psoriasis Area and Severity Index (PASI), body surface area, and Physician’s Global Assessment scores.
The use of TM can provide additional care that may not usually be available, such as internet-based cognitive behavioral therapy and mental health care. The IPC has a platform for discussing best practice treatment approaches and what teledermatology can offer to patients; they acknowledged that, in certain situations, TM is not the optimal approach. Figure 3 highlights situations in which an in-person visit is preferred.
Figure 3. Situations in which an in-person visit is preferred, according to the IPC working group*
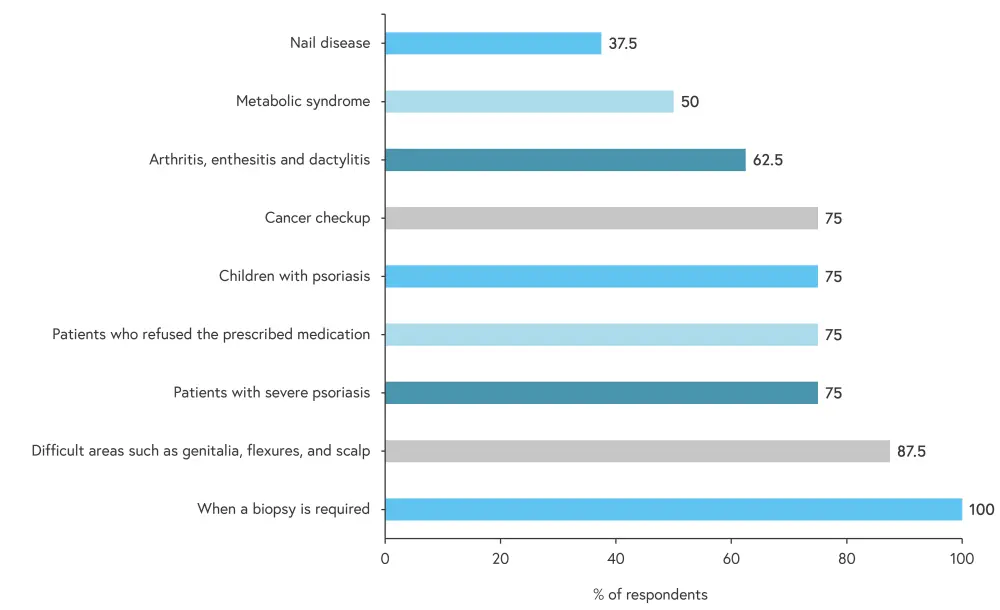
*Adapted from El Komy, et al.1
Does TM provide opportunities for treatment innovation?
Early diagnosis, which is integral to psoriasis treatment, can be facilitated by improving access to care with TM. However, using TM for diagnosis follow-up care needs optimization.
Using pictures and automated PASI scoring
Photography is already used in dermatology to track the progression of disease and for educational purposes. As technology has improved over time, the quality of photos has also improved; however, this depends on the equipment used. Figure 4 highlights some of the key recommendations for patients who need to take photos as part of their care routine.
Figure 4. Photography recommendations for patients with psoriasis using TM*
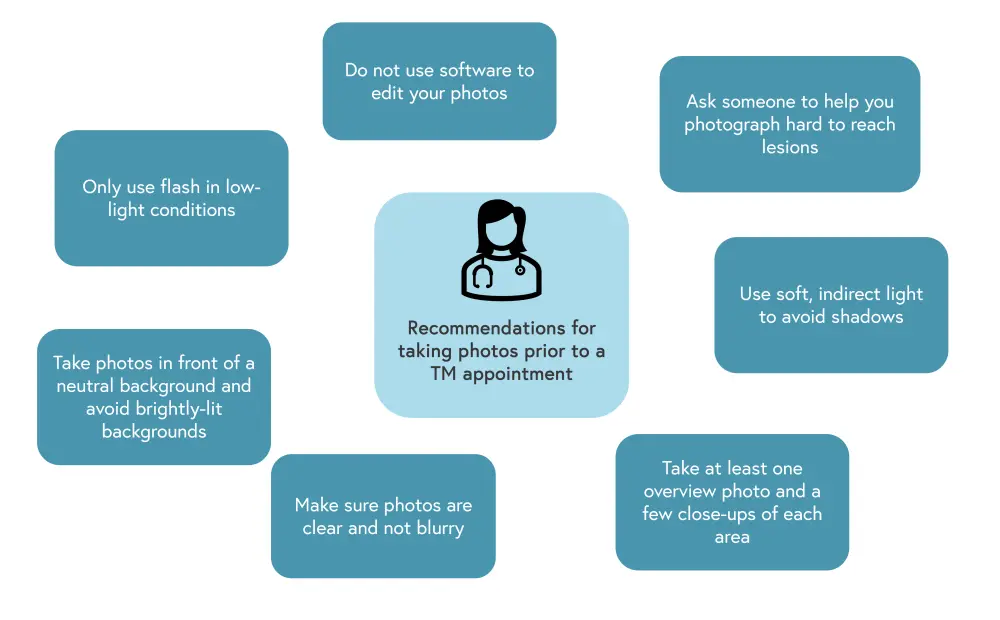
*Adapted from El Komy, et al.1
Artificial intelligence (AI) has the potential to guide and assist patients in taking photos. As a fairly recent development in healthcare, it has likely not yet been used in teledermatology; however, AI has been implemented to support PASI and body surface area measurements. Here, automation is beneficial as taking these measurements can take time in clinical practice. The IPC suggest that the development of smartphone applications that utilize AI could be useful in real-world settings.
Which treatments can be initiated and continued by TM?
The working group members, excluding one member who no longer regularly treats patients, voted on which treatment initiation and continuation decisions may be determined using TM (Figure 5). All members agreed that TM could be used to make treatment initiation and continuation decisions for topical treatment. No other medication reached 100% consensus, but three other treatments, including apremilast and biologic agents, were considered suitable for continuation using TM by the entire panel.
Figure 5. Suitable treatments for initiation and continuation by TM, according to the IPC working group*
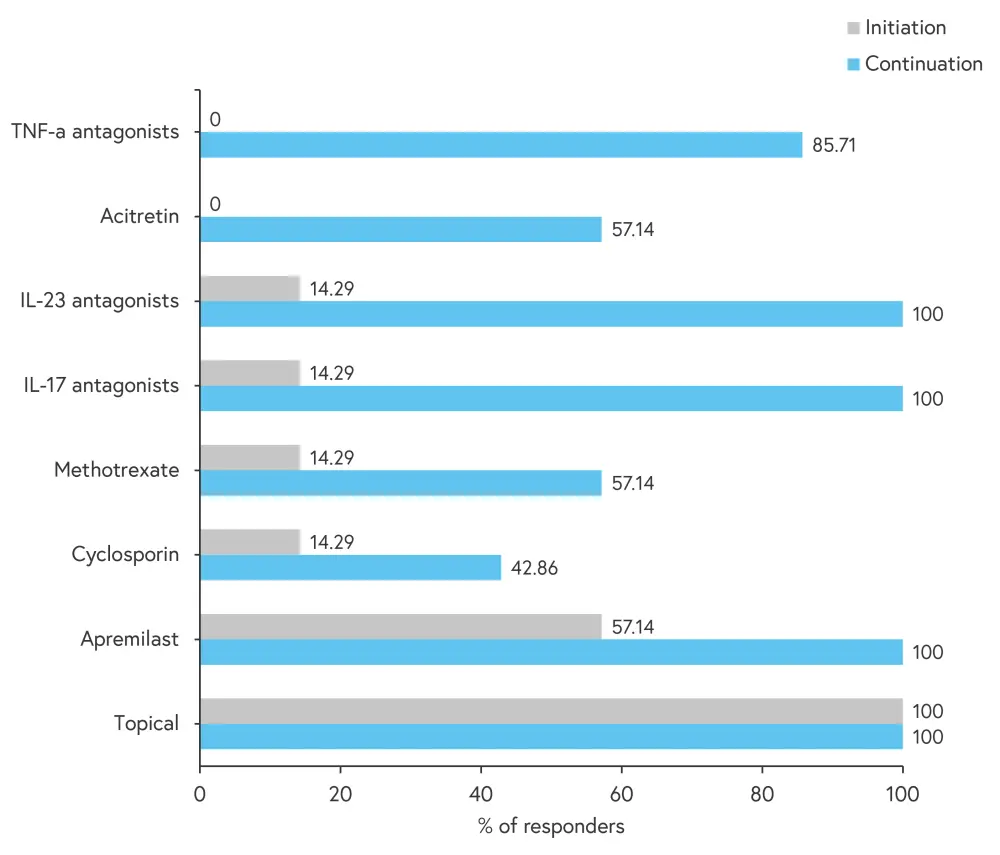
*Adapted from El Komy, et al.1
In summary, the IPC agreed at teledermatology can effectively be used to initiate and continue topical therapies and to continue treatment with biologics.
Access to care in underserved areas
By increasing the number of available consultants and reducing waiting times, teledermatology has the potential to benefit medically disadvantaged populations. Suboptimal specialized care can impact rural or difficult to reach communities and those experiencing financial difficulties, this may be due to shortage of dermatologists or lack of access. The IPC state that teledermatology should aim to improve patient care based on the needs of currently underserved patients.
Conclusion
The IPC working group has determined that teledermatology can play an important role in treating patients with psoriasis. However, there are instances where teledermatology is not suitable, such as the management of psoriasis in special areas; effective TM may also depend on the cultural expectations of patients. Medical education should provide guidance on TM practices, including its benefits and limitations. The IPC plan to provide a forum for physicians to discuss best practice for utilizing both teledermatology and in-person treatment to improve patient care.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with psoriatic arthritis do you see per month?

