All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The pso Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the pso Hub cannot guarantee the accuracy of translated content. The pso and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The PsOPsA Hub is an independent medical education platform, supported by educational grants. We would like to express our gratitude to the following companies for their support: UCB, founding supporter. The funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View psoriasis and psoriatic arthritis content recommended for you
Updated GRAPPA treatment guidelines for psoriatic arthritis
Do you know... Which of the following options is not a domain of PsA?

The Good Care Campaign for Psoriatic Arthritis
Psoriatic arthritis (PsA) affects both the joints and skin of individuals who may also have psoriasis.1 Approximately 33% of individuals with psoriasis experience joint pain, stiffness, and swelling in the joints, leading to irreversible damage if left untreated.2 PsA can also trigger inflammation in various parts of the body, such as the eyes, heart, lungs, and kidneys.3
Unfortunately, there is a lack of understanding about the nature and impact of living with this disease, including its manifestations and related symptoms.1 Despite PsA being the second most common inflammatory joint disease,4 causing significant stiffness, swelling, and pain that often leads to disability,5 there remains a lack of awareness regarding the immense burden it places on individuals and society.1
Access to adequate care and treatment6
The management of PsA often involves uncertainties, making it difficult to achieve successful outcomes for individuals affected by the disease. However, recent guidelines, such as the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA) guidelines, include the implementation of treat-to-target (T2T) strategies. T2T approaches have been widely accepted in the treatment of other forms of arthritis and other inflammatory diseases, but they may not broadly be used in the management of PsA. The GRAPPA guidelines consider various domains of symptoms and tailor treatment targets accordingly. Many individuals living with PsA face significant challenges, including the inability to work due to this debilitating condition and the need for frequent and costly treatments.
CALL TO ACTION
IFPA’s Good Care Campaign for Psoriatic Arthritis is raising awareness among healthcare providers to adopt T2T strategies in the management of PsA. IFPA advocates for clearer guidelines and further research to support effective treatment plans for individuals with PsA. IFPA also raises awareness about the impact of PsA on individuals' lives and the broader community. The personal and financial burden of PsA cannot be overlooked. The frequent need for medical appointments, medications, and specialized treatments can place a heavy strain on individuals and their families. Moreover, the societal impact, including lost productivity and increased healthcare costs, further highlights the urgency for better treatment support and resources.
Recognizing comorbidities and the need for multidisciplinary care6
PsA is often associated with several comorbidities, including depression, anxiety, diabetes, and inflammatory bowel disease. These associated conditions can significantly impact an individual's quality of life. Therefore, it is crucial to consider the presence of comorbidities when formulating treatment plans to provide the best possible care and prevent or treat these associated conditions. The GRAPPA guidelines support decision-making and take into account comorbidities (Figures 1 and 2).
Figure 1. Treatment schema*
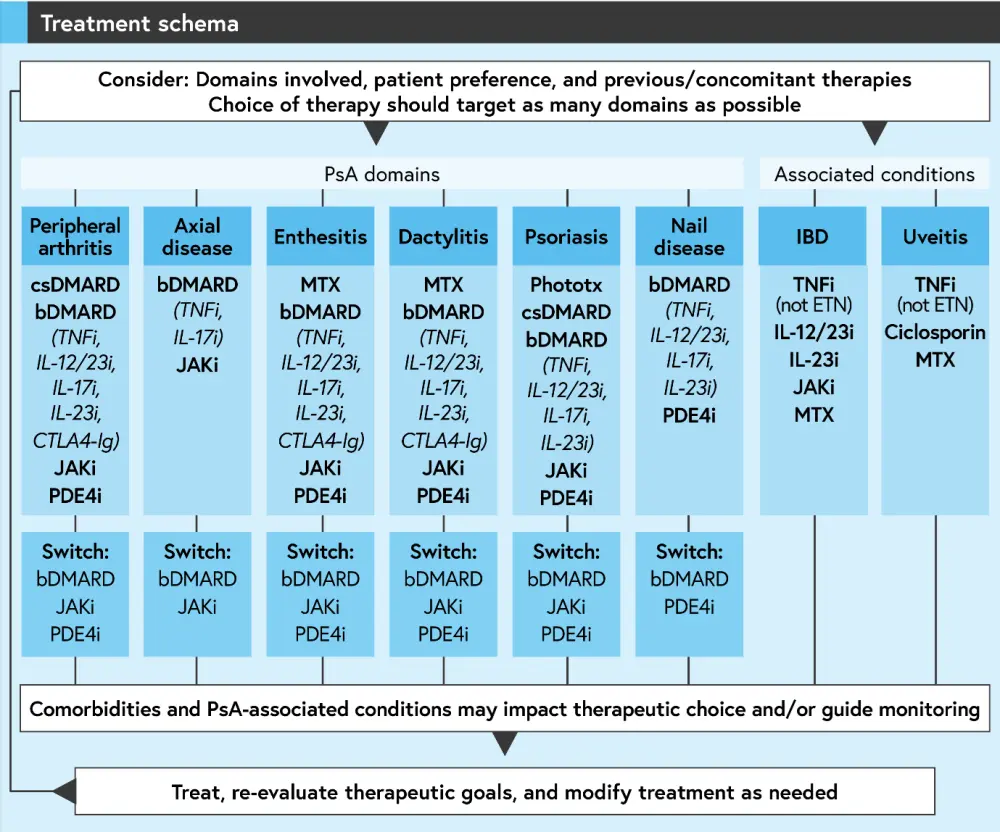
*Adapted from Coates, et al.6
Figure 2. Summary recommendations for PsA treatment in the case of comorbidities*
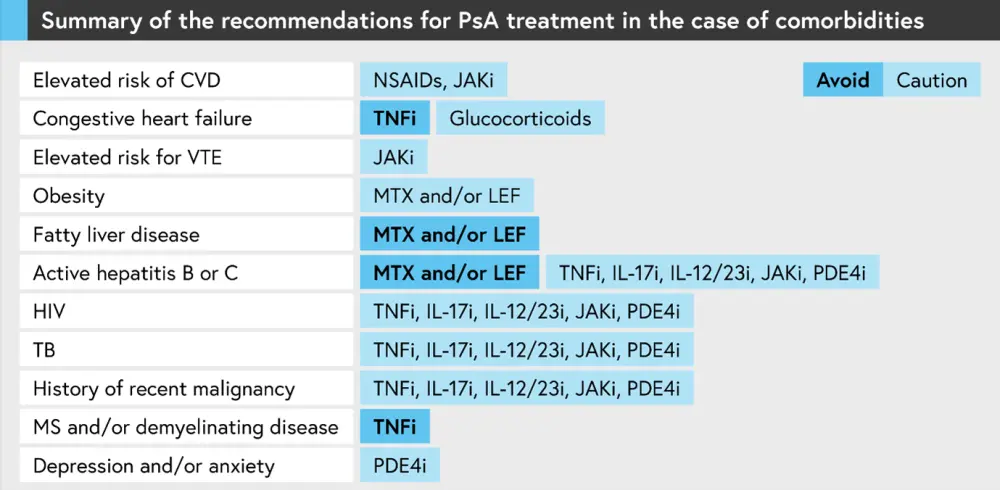
*Adapted from Coates, et al.6
CALL TO ACTION
Breaking the stigma surrounding mental health and PsA by integrating mental health and wellbeing support for care is crucial. Encouraging healthcare providers to connect people living with PsA to patient organizations is important. IFPA advocates for comprehensive care that addresses not only PsA but also the associated comorbidities, and supports research efforts to better understand the connections between PsA and these conditions.
Addressing inclusive and comprehensive care, including sexual and reproductive concerns6
Women of reproductive age and their partners may experience unique symptoms that require individualized treatment options. It is essential for healthcare providers to have open conversations with patients, discussing their needs and exploring different therapy options until they find what works best for them.
CALL TO ACTION
IFPA calls for inclusive and comprehensive care for individuals with PsA, including addressing sexual health and reproductive concerns. IFPA advocates for healthcare providers to proactively engage in conversations about these topics and provide appropriate resources and support
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with plaque psoriasis do you see per month?

