All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The pso Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the pso Hub cannot guarantee the accuracy of translated content. The pso and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The PsOPsA Hub is an independent medical education platform, supported by educational grants. We would like to express our gratitude to the following companies for their support: UCB, for website development, launch, and ongoing maintenance; UCB, for educational content and news updates. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View psoriasis and psoriatic arthritis content recommended for you
The safety and efficacy of brepocitinib in patients with PsA and PsO: Results from a phase IIb trial
There are currently multiple approved treatments for patients with psoriatic arthritis (PsA).1 In recent years, there have been several Janus kinase (JAK) inhibitors approved for use in patients with PsA. JAK inhibitors can prevent inflammation in PsA through blockade of interferon signaling.1
Brepocitinib is a JAK1 and TYK2 inhibitor which has previously shown superiority in improving Psoriasis Area and Severity Index (PASI) scores compared with placebo in clinical trials.1 Here, we report the results of a randomized, placebo-controlled phase Iib trial of brepocitinib at three doses in patients with active psoriasis and PsA.
Study design1
A total of 218 patients across 11 countries were randomized and treated in this study. The study design is shown in Figure 1. There were three dosing cohorts of brepocitinib, plus a placebo cohort. Patients were allowed to continue treatment during the study with non-steroidal anti-inflammatory drugs, COX-2 inhibitors, or prednisone if receiving a stable dose.
Figure 1. Study design*
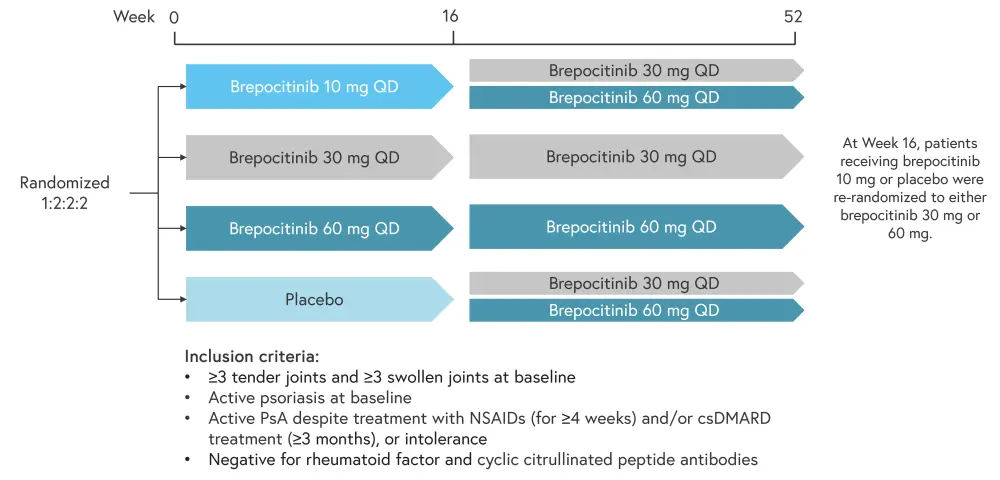
csDMARD, conventional synthetic disease-modifying antirheumatic drug; NSAID, non-steroidal anti-inflammatory drug; PsA, psoriatic arthritis; QD, once daily.
*Adapted from Mease, et al.1
The primary endpoint of this study was the percentage of patients who achieved a 20% improvement in American College of Rheumatology response (ACR20) at Week 16. Key secondary endpoints included ACR70, 75% improvement in PASI (PASI75), and PASI90 responses.
Results1
Of the 218 patients randomized, one patient in the brepocitinib 30 mg cohort did not receive any treatment and was excluded from efficacy and safety analyses. Up to Week 16 and between Weeks 20 and 52, 15 and 35 participants discontinued treatment, respectively. Patient characteristics at baseline were similar across treatment groups, as shown in Table 1. The majority of patients in each treatment group were receiving csDMARDs, methotrexate, and/or NSAIDs and all patients apart from one in the brepocitinib 60 mg group were White.
Table 1. Baseline patient characteristics*
|
BMI, body mass index; csDMARD, conventional synthetic disease-modifying antirheumatic drug; DAPSA, Disease Activity Index for PsA; HAQ-DI, Health Assessment Questionnaire – Disability Index; NSAID, non-steroidal anti-inflammatory drug; PASDAS, Psoriatic Arthritis Disease Activity Score; PASI, Psoriasis Area and Severity Index; QD, once daily; SJC, swollen joint count; TJC, tender joint count. *Adapted from Mease, et al.1 |
||||
|
Characteristic |
Brepocitinib |
Placebo (n = 67) |
||
|---|---|---|---|---|
|
10 mg QD |
30 mg QD |
60 mg QD (n = 60) |
||
|
Mean age, years |
47.8 |
45.9 |
48.7 |
48.2 |
|
Male, % |
54.8 |
46.7 |
43.3 |
46.3 |
|
Mean BMI, kg/m2 |
28.7 |
30.2 |
28.7 |
28.8 |
|
Mean PASDAS, n |
5.7 |
5.7 |
5.4 |
5.7 |
|
Mean DAPSA, n |
39.9 |
38.6 |
37.2 |
37.9 |
|
Mean HAQ-DI, n |
1.1 |
1.1 |
1.0 |
1.1 |
|
Mean TJC, n |
16.5 |
16.6 |
17.3 |
16.0 |
|
Mean SJC, n |
11.1 |
9.6 |
9.3 |
9.8 |
|
Mean PASI, n |
11.9 |
10.5 |
10.8 |
11.2 |
|
Medication use at |
|
|
|
|
|
csDMARDs |
74.2 |
66.7 |
83.3 |
73.1 |
|
Methotrexate |
67.7 |
63.3 |
76.7 |
71.6 |
|
NSAIDs |
67.7 |
53.3 |
56.7 |
50.7 |
|
Oral steroids |
16.1 |
10.0 |
15.0 |
16.4 |
|
Topical |
3.2 |
3.3 |
1.7 |
0 |
Safety
By Week 16, 119 patients had experienced a treatment-emergent adverse event. The rate of adverse events is shown in Figure 2.
Figure 2. Rate of TEAEs, SAEs, and infections at A Week 16 and B Week 52*
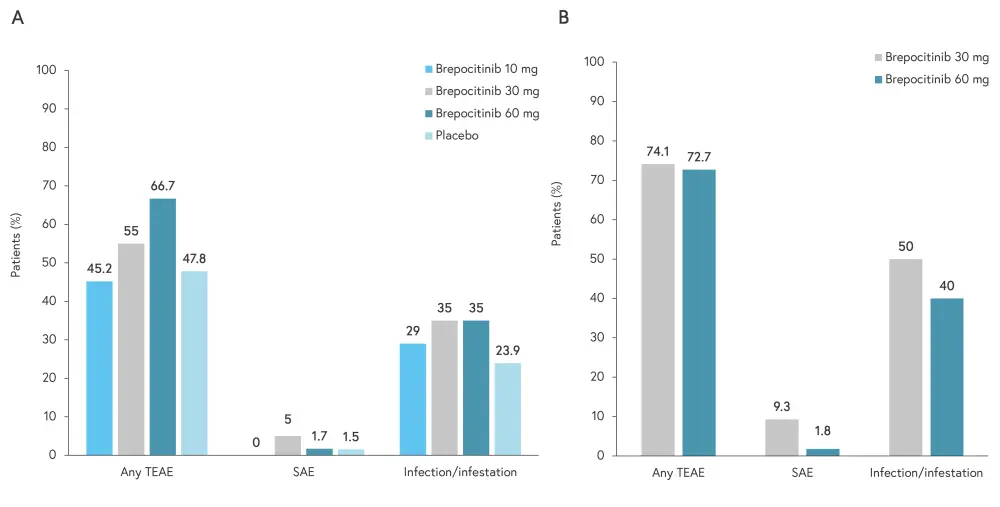
SAE, serious adverse event; TEAE, treatment-emergent adverse event.
*Adapted from Mease, et al.1
Efficacy
Significantly more patients in the brepocitinib 30 mg (p = 0.0197) and 60 mg (p = 0.0006) groups achieved ACR20 at Week 16 compared with placebo. ACR20 responses at Week 16 are shown in Figure 3, alongside other secondary endpoints at Week 16.
Figure 3. ACR20 and secondary efficacy endpoints at Week 16*
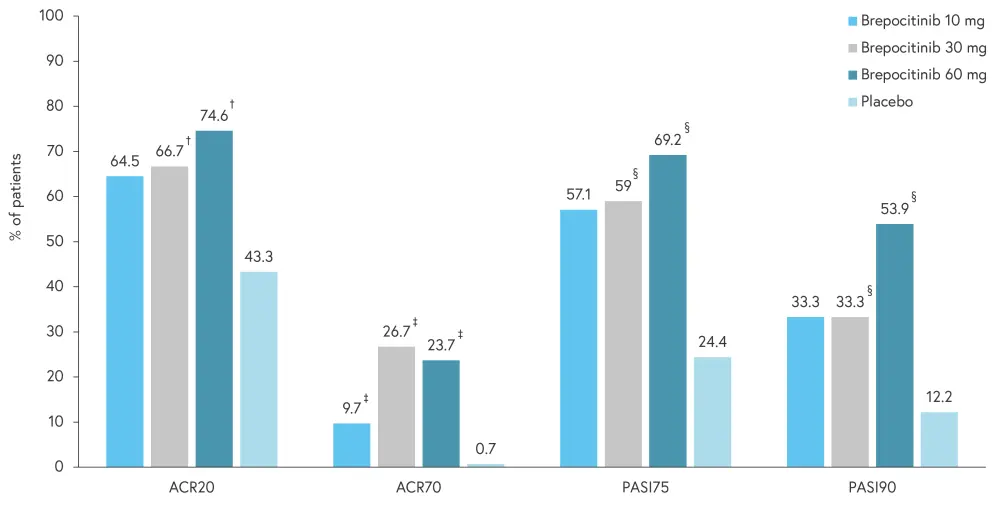
ACR20, 20% improvement in the American College of Rheumatology response; ACR70, 70% improvement in ACR response; PASI75, 75% improvement in Psoriasis Area and Severity Index; PASI90, 75% improvement in PASI.
*Adapted from Mease, et al.1
†Indicates statistical significance vs placebo using a 2-sided adjusted p < 0.1 based on Dunnett’s method.
‡Indicates statistical significance vs placebo using informal testing without overall family-wise type-I error rate controlled, 2-sided p < 0.1 based on the normal approximation for binomial proportions.
§Indicates statistical significance vs placebo, 2-sided p < 0.1 based on the normal approximation for binomial proportions, using formal testing with overall family-wise type-I error rate controlled.
Significant improvements in patient-reported outcomes, such as Health Assessment Questionnaire – Disability Index, were also observed in cohorts treated with brepocitinib 30 mg and 60 mg compared with placebo. The ACR20, ACR70, PASI75, and PASI90 responses were generally sustained up to Week 52 in the brepocitinib 30 mg and 60 mg cohorts; however, improvements were observed more frequently in the 30 mg cohort.
Conclusion
This phase II study demonstrated that brepocitinib can be used safely in patients with psoriasis and concurrent PsA at a range of doses.1 Treatment with brepocitinib 30 mg and 60 mg led to significant improvements in ACR and PASI responses at Week 16.1 Patient reported outcomes were also generally improved at Week 16 in the 30 mg and 60 mg groups, which may indicate an improvement in quality of life. At all doses, brepocitinib was generally well tolerated and the majority of adverse events were mild to moderate. This study was limited by a lack of diversity in the study population, with all but one patient being White, and by the lack of a placebo control past Week 16.1 Therefore, additional long-term, placebo-controlled studies in both psoriasis and PsA would be beneficial.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with psoriatic arthritis do you see per month?

