All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The pso Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the pso Hub cannot guarantee the accuracy of translated content. The pso and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The PsOPsA Hub is an independent medical education platform, supported by educational grants. We would like to express our gratitude to the following companies for their support: UCB, for website development, launch, and ongoing maintenance; UCB, for educational content and news updates. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View psoriasis and psoriatic arthritis content recommended for you
Role of gut bacterial metabolites in PsO and PsA
Do you know... Evidence from a review by Lai et al. suggests that western diet leads to a reduction in short- chain fatty acid protective properties. Which one of the following statements is false regarding the reduction in short- chain fatty acid protective properties?
Psoriasis (PsO) is a chronic inflammatory skin condition mediated by the immune system which increases the risk of developing other health conditions, including obesity, diabetes mellitus, and cardiovascular disease.1 While PsO currently remains incurable, treatment options are directed at the management of physical and psychological symptoms. Gut dysbiosis has been established as a key component in the pathogenesis of PsO, in particular the interaction between gut microbiota and the host via bacteria-derived metabolites.1
Here, we summarize a recent review by Lai et al published in Journal of Investigative Dermatology outlining the role of bacteria-derived metabolites in the functioning of the immune system and their association with PsO.
Gut bacteria-derived metabolites
- Studies have shown patients with PsO have a noticeably reduced gut bacterial diversity.
- The mechanisms underlying how the gut microbiota influences the host are complex and multifaceted; however, studies have shown a substantial impact of bacteria-derived metabolites on several host biological processes and the overall health (Figure 1).
Figure 1. Impact of bacteria-derived metabolites on host biological processes*
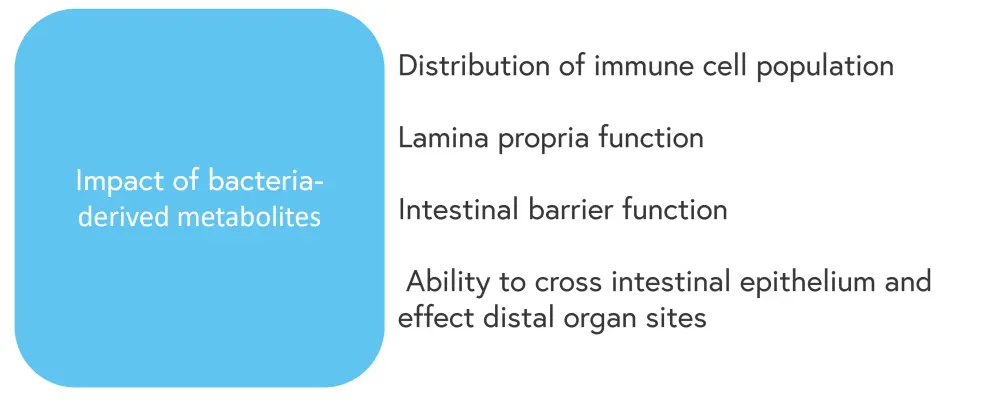
*Adapted from Lei, et al.1
Short-chain fatty acids
- Short-chain fatty acids (SCFAs) are produced via the fermentation of dietary fiber and resistant starches by anaerobic bacteria.
- SCFAs promote immunoglobulin A responses and the induction of genes encoding mucin protein and tight junction components, preventing gut barrier failure.
- They also influence the release of reactive oxygen species, cytokines, and immune cell chemotaxis promoting host protection.
- Studies suggest that SCFA and SFCA-producing bacteria have a role in modulating T-cell function and stimulating the production of retinoic acid, enhancing the differentiation of regulatory T cells.
- Western diets, which are often high in fat and low in dietary fiber, lead to a reduction in several biological factors associated with SCFA synthesis:
- Fewer SCFA precursors in the gut
- Lower levels of genes involved in SCFA bacterial metabolic pathways and secreting bacteria
- Collectively, this leads to a reduction in SCFA protective properties and increased pro-inflammatory effects (Figure 2)
- Considering these factors, SCFA supplementation represents a potential therapeutic option for patients with PsO.
Figure 2. Impact of reduced levels of SCFAs on the host*
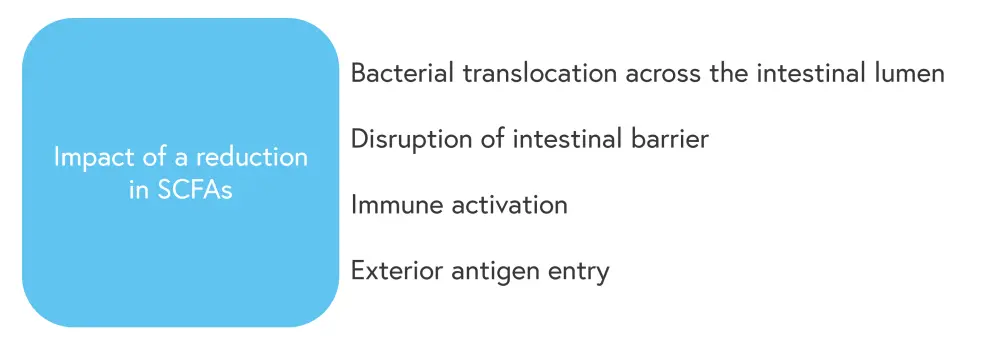
SCFA, short chain fatty acid.
*Adapted from Lei, et al.1
Bile acids
- Bile acids (BA) are cholesterol-derived natural surfactants produced in the liver and secreted in the duodenum.
- A small proportion of these molecules undergo bacterial transformation to secondary BAs in the colon.
- BAs influence gut microbial composition by promoting the growth of BA metabolizing bacteria and inhibiting the growth of other BA-sensitive bacteria.
- BAs also plays a role in immune homeostasis and adaptive immunity, specifically the T helper 17/ T regulatory cell balance, insulin resistance, cardiovascular disease, neurodegenerative disease, tumorigenesis, and aging.
- BAs are also becoming increasingly recognized as an important signaling molecule in PsO.
- A longitudinal study showed patients with PsO had decreased serum levels of secondary BAs and were at higher risk of progression to psoriatic arthritis.
- BA supplementation is recognized as a potential therapeutic option for patients with PsO.
- A study reported that 80% of patients experienced a complete resolution of symptoms with dehydrocholic acid supplementation vs 25% of patients treated with conventional therapy.
Tryptophan metabolites
- Tryptophan is one of nine essential amino acids, of which a small proportion is catabolized in the colon producing indole derivatives.
- The influences of indole derivatives on host biological functions are highlighted in Figure 3.
- While there is a weak link between tryptophan metabolites and PsO, the topical administration of the aryl hydrocarbon receptor agonist and tapinarof showed efficacy during treatment.
Figure 3. Impact of indole derivatives on the host*
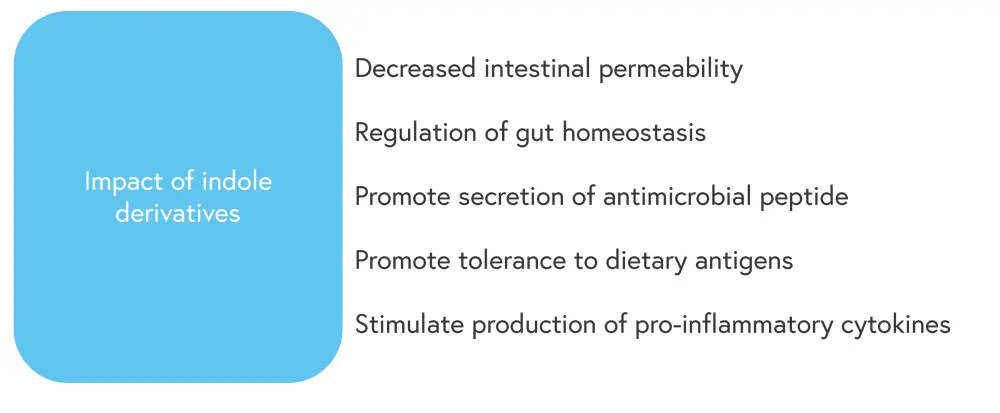
*Adapted from Lei, et al.1
Trimethylamine N-oxide
- Trimethylamine N-oxide is derived from dietary phosphatidylcholine and has a role in the pathogenesis of atherosclerosis and cardiovascular disease.
- Patients with psoriasis have a higher risk of developing cardiovascular disease.
- A study showed significantly higher fasting plasma trimethylamine N-oxide levels in patients with PsO compared with healthy controls.
- Higher levels of trimethylamine N-oxide were significantly correlated with measures of PsO disease activity for both skin and peripheral joints.
Conclusion
The potential of gut symbionts as preventative and therapeutic targets has been greatly enhanced by the growing body of research on the role of gut dysbiosis in the pathogenesis of PsO. While molecular mechanisms remain poorly understood, it is becoming increasingly clear that bacterial-derived metabolites play a key role in the regulation of host innate and adaptive immunity. Results from current studies show substantial variation regarding the role of the microbiome in PsO and psoriatic arthritis. Further translational research on gut bacterial metabolites and robust randomized trials are warranted.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with psoriatic arthritis do you see per month?

