All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The pso Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the pso Hub cannot guarantee the accuracy of translated content. The pso and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The PsOPsA Hub is an independent medical education platform, supported by educational grants. We would like to express our gratitude to the following companies for their support: UCB, for website development, launch, and ongoing maintenance; UCB, for educational content and news updates. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View psoriasis and psoriatic arthritis content recommended for you
Mental health comorbidities associated with psoriasis
Do you know... In a recent study by Chu et al., which of the following was identified to have a bidirectional causal relationship with psoriasis?
There is a high prevalence of mental health comorbidities in individuals with chronic psoriasis, including depression, anxiety, and suicidality. The causal relationship between the disease burden of psoriasis and mental health comorbidities is unclear, though studies suggest that there may be a link between psychosocial stress and exacerbation of psoriasis symptoms.1
Here, we summarize key data from a study investigating the cause-effect relationships between psoriasis and mental health comorbidities.
Study design1
- This was a bidirectional two-sample, Mendelian randomization (MR) study utilizing summary statistics from publicly available comprehensive genome-wide association studies of:
- psoriasis (n = 306,123);
- broad depression (n = 500,199);
- major depressive disorder (n = 173,005);
- anxiety (n = 17,310); and
- suicide attempts (n = 50,264).
- Single nucleotide polymorphisms associated with exposure at a genome-wide significance of p < 5 × 10-8, were selected for psoriasis, broad depression, and major depressive disorder, with the threshold for anxiety and suicide attempt being p < 5 × 10-6.
- The random-effects inverse-variance weighted (IVW) model was used as the main analysis, along with several complementary statistical methods.
- Significant evidence for association between disease burden and mental health comorbidities was regarded as associations with p < 0.00625.
Findings1
The forward-direction MR analyses suggested that psoriasis was significantly associated with an increased risk of broad depression but only suggestively associated with risk of major depressive disorder (Figure 1).
Figure 1. Association of psoriasis with the risk of A broad depression and B major depressive disorder in forward MR analyses*
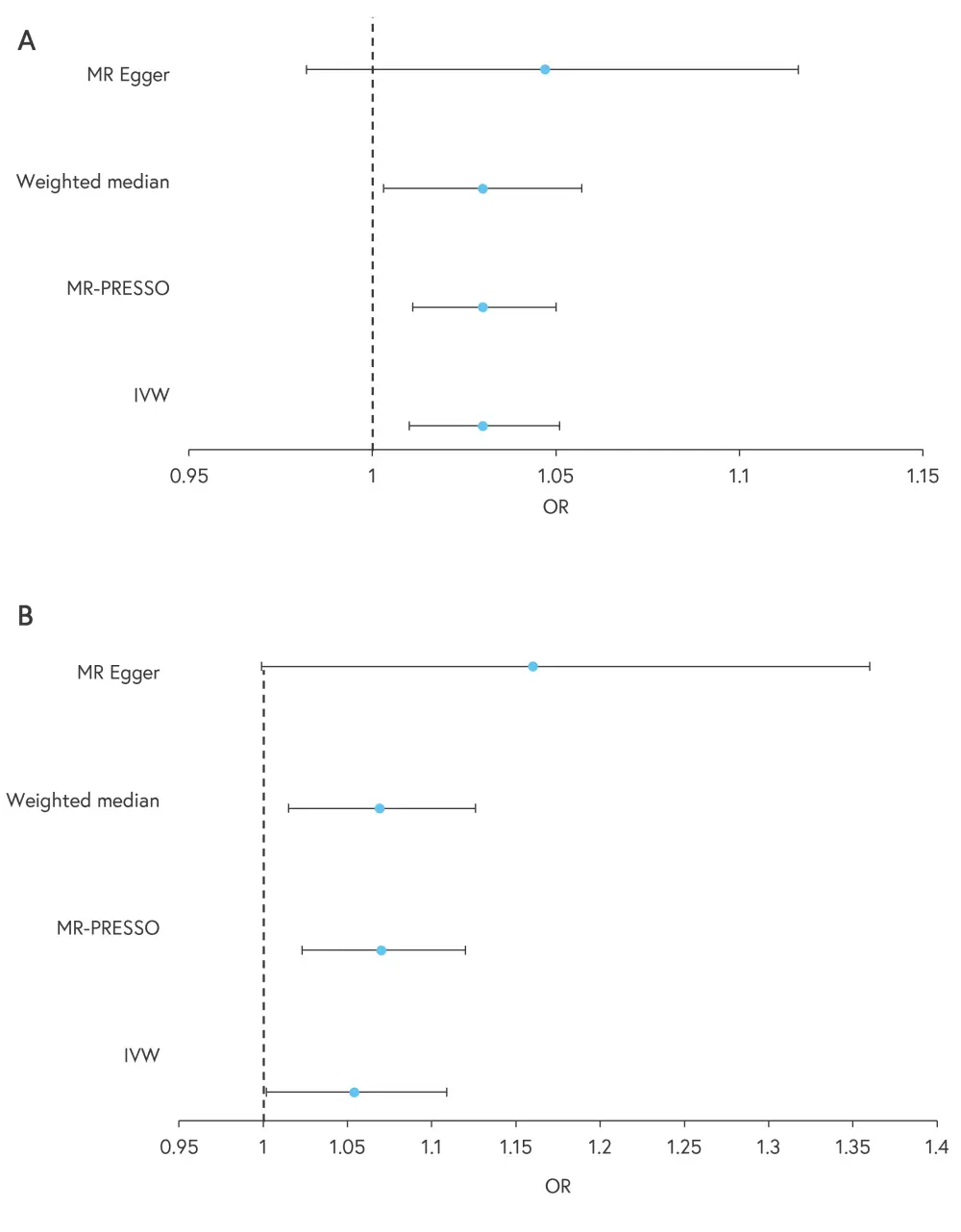
IVW, inverse-variance weighted model; MR, Mendelian randomization; MR-PRESSO, MR-Pleiotropy residual sum and outlier; OR, odds ratio.
*Adapted from Chu, et al.1
Psoriasis was found not to be significantly associated with the risk of anxiety or suicidality (Table 1).
Table 1. Association of psoriasis with the risk of anxiety in forward MR analysis*
|
MR, Mendelian randomization; IVW, effects inverse-variance weighted model; MR-PRESSO, MR-Pleiotropy residual sum and outlier. |
||||
|
Model |
Odds ratio (anxiety) |
p value |
Odds ratio (suicidality) |
p value |
|---|---|---|---|---|
|
IVW |
1.109 |
0.160 |
1.014 |
0.648 |
|
MR-PRESSO |
1.109 |
0.178 |
1.014 |
0.654 |
|
Weighted median |
1.106 |
0.221 |
1.015 |
0.721 |
|
MR Egger |
1.430 |
0.080 |
1.011 |
0.845 |
The reverse-direction MR analyses suggested that psoriasis was significantly associated with an increased risk of broad depression and major depressive disorder (Figure 2).
Figure 2. A Broad depression and B major depressive disorder associated with risk of psoriasis in reverse MR analyses*
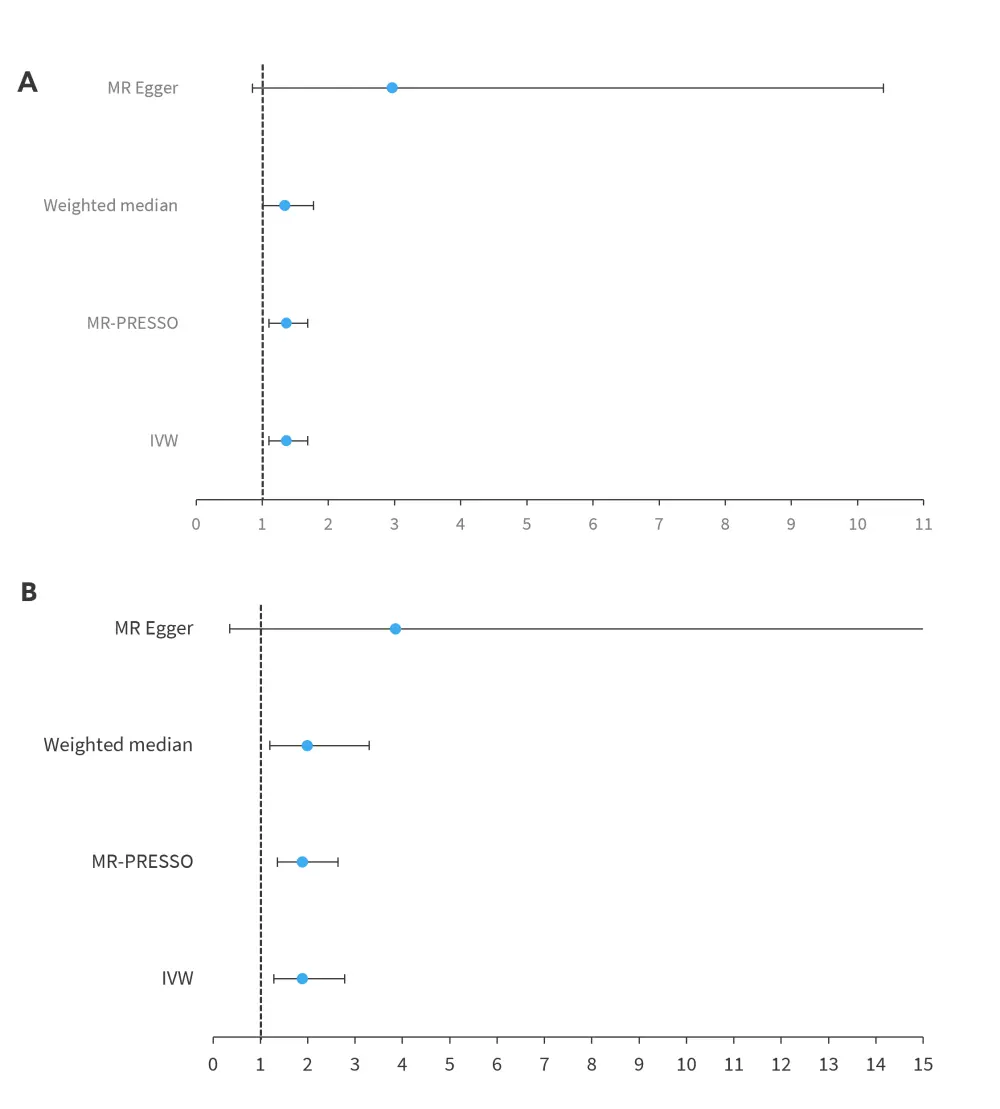
MR, Mendelian randomization; IVW, effects inverse-variance weighted model; MR-PRESSO, MR-Pleiotropy residual sum and outlier; OR, odds ratio.
*Adapted from Chu, et al.1
There was no evidence for a causal effect of anxiety or suicidality on an increased risk of psoriasis.
Conclusion1
The results of this study suggest a causal link between psoriasis and the risk of depression and vice versa. This bidirectional relationship warrants further investigation. Screening for depression in patients with psoriasis, along with appropriate management, may lead to improved clinical outcomes.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with psoriatic arthritis do you see per month?

