All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The pso Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the pso Hub cannot guarantee the accuracy of translated content. The pso and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The PsOPsA Hub is an independent medical education platform, supported by educational grants. We would like to express our gratitude to the following companies for their support: UCB, for website development, launch, and ongoing maintenance; UCB, for educational content and news updates. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View psoriasis and psoriatic arthritis content recommended for you
Editorial theme | Points to consider in the development of PsA in individuals with psoriasis from the EULAR task force
In approximately 70% of individuals with psoriatic arthritis (PsA), psoriasis occurs first and can precede PsA development by decades.1 Skin involvement in psoriasis could be predictive of increased risk of PsA occurrence.1 Identifying predictors for PsA development could allow for earlier treatment, or prevention of PsA in these individuals.1
It has been suggested that there are three stages between psoriasis and PsA development, as shown in Figure 1.2 Building on this, the European Alliance of Associations for Rheumatology (EULAR) developed a task force to produce guidance for clinical trials focused on the prevention of PsA, and the management of individuals at risk of PsA.1 Here, we discuss the main guidance provided from the task force.
Figure 1. Stages from psoriasis to early PsA*
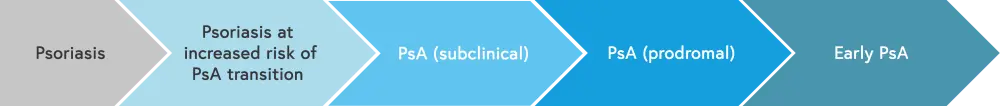
PsA, psoriatic arthritis.
*Data from Scher, et al.2
Findings1
The EULAR task force comprised 29 members: 21 rheumatologists, five dermatologists, two patient partners, and one healthcare professional.
The task force had three objectives:
- Defining the main features present in individuals who transition from psoriasis to PsA
- Characterizing the phenotype of new-onset PsA
- Identifying the stages of progression from psoriasis to PsA, relevant to PsA prevention
The method of developing these recommendations followed EULAR standardized operating procedures, using a consensual approach and systemic literature research. The task force developed five overarching principles, as shown in Figure 2.
Figure 2. Overarching principles*
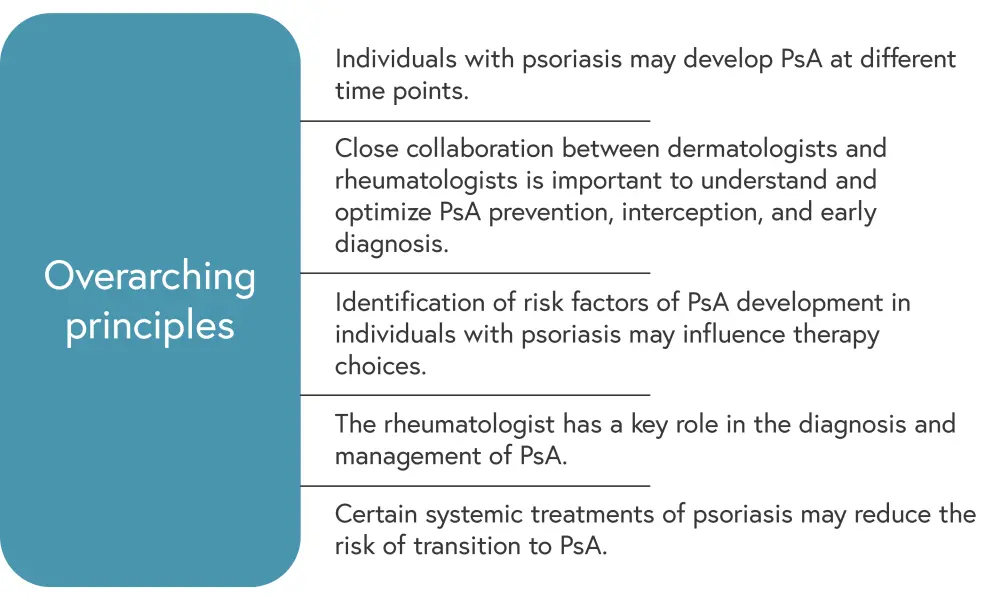
LoA, level of agreement; PsA, psoriatic arthritis.
*Adapted from Zabotti.1
The task force also identified points to consider for clinical trials on the prevention or interception of PsA and on the management of psoriasis in individuals at risk of PsA. These points were rated on the level of evidence (LoE) and level of agreement (LoA) for each point. Figure 3 illustrates the points to consider with the highest LoE (Level 5). Additional points to consider included:
- In clinical trials on prevention and interception of PsA:
- Imaging in individuals with psoriasis could be used to identify those at risk of PsA (LoE, 3b; LoA, 9.1).
- For the management of psoriasis in individuals at risk of PsA,
-
- arthralgia in individuals with psoriasis should be considered as a short-term predictor of PsA development (LoE, 3a; LoA, 9.2);
- in individuals with psoriasis, joint and entheseal pain and functional limitation should be enquired about regularly and referral to a rheumatologist should be considered if present (LoE, 3b; LoA, 9.3);
- imaging abnormalities in the absence of musculoskeletal symptoms should be considered carefully to ensure appropriate treatment (LoE, 3b; LoA, 9.5); and
- individuals with psoriasis and obesity, nail disease, and/or extensive psoriasis should be considered at higher risk of PsA development long term (LoE, 3a; LoA, 9.3).
Figure 3. Points to consider with high LoE*
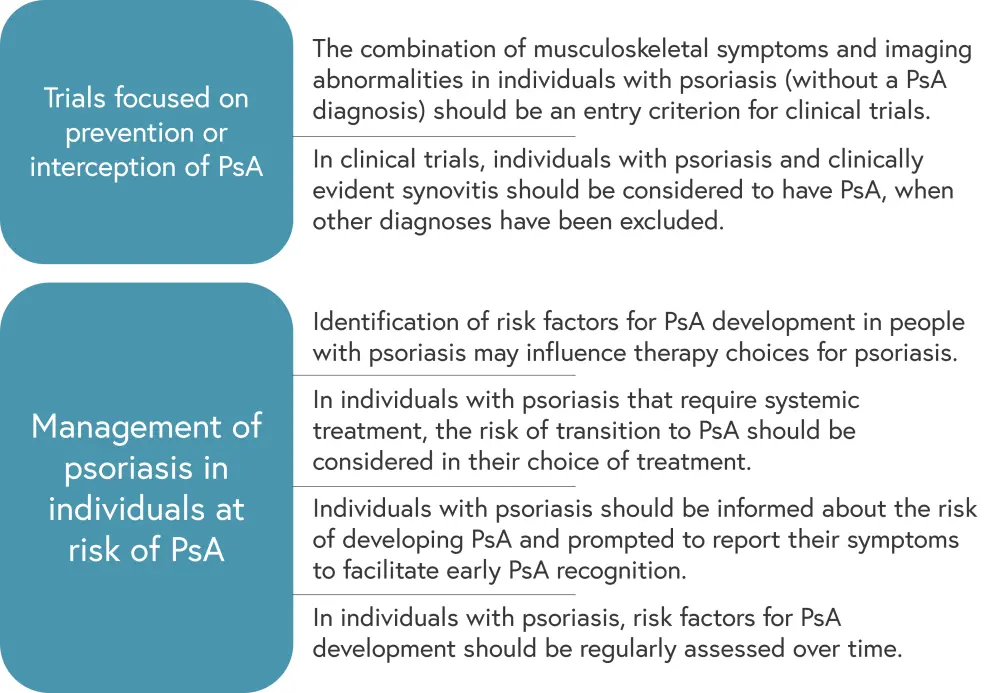
LoA, level of agreement; LoE, level of evidence; PsA, psoriatic arthritis.
*Adapted from Zabotti.1
Finally, the task force developed definitions for the phases of PsA development in individuals with psoriasis; this is shown in Figure 4.
Figure 4. Definitions of the phases of PsA development for use in clinical trials*
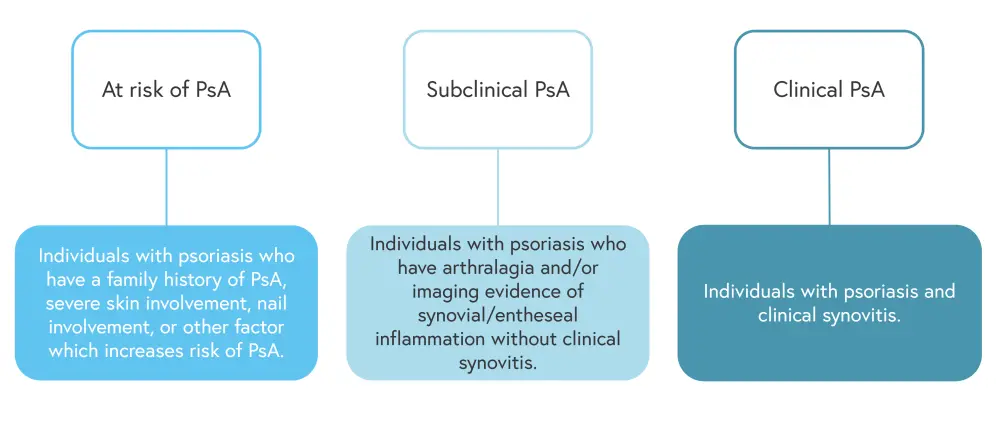
PsA, psoriatic arthritis.
*Data from Zabotti.1
Conclusion
The recommendations of the EULAR task force provide an evidence-based framework for use in clinical trials on the risk of PsA development and for the management of individuals with psoriasis who may be at risk of PsA.1 However, Zabotti highlighted that in patients with psoriasis without evidence of muscloskeletal involvement, imaging techniques such as ultrasound and magnetic resonance imaging should only be used in the clinical trial setting; there is currently no evidence that imaging can be used for risk stratification in PsA.1 Therefore, it is important to differentiate between points to consider for clinical trials and points to consider for the management of individuals with psoriasis at risk of PsA.1
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with plaque psoriasis do you see per month?

