All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The pso Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the pso Hub cannot guarantee the accuracy of translated content. The pso and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The PsOPsA Hub is an independent medical education platform, supported by educational grants. We would like to express our gratitude to the following companies for their support: UCB, for website development, launch, and ongoing maintenance; UCB, for educational content and news updates. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View psoriasis and psoriatic arthritis content recommended for you
Case study | upadacitinib in a pediatric patient with nail psoriasis
Nail psoriasis is a common manifestation in patients with psoriatic disease, affecting ~80% of individuals with psoriasis.1 Nail psoriasis can be indicative of more severe disease, and can be predictive of psoriatic arthritis development.1 Nail psoriasis can also impact quality of life, causing pain and functional impairment.1 Here, we discuss a case study of a pediatric patient with nail psoriasis who received treatment with upadacitinib.
This is a case study of a 13-year-old patient who has been affected by progressive nail distortion for 8 years.1 The patient history is given in Figure 1.
Figure 1. Patient history*
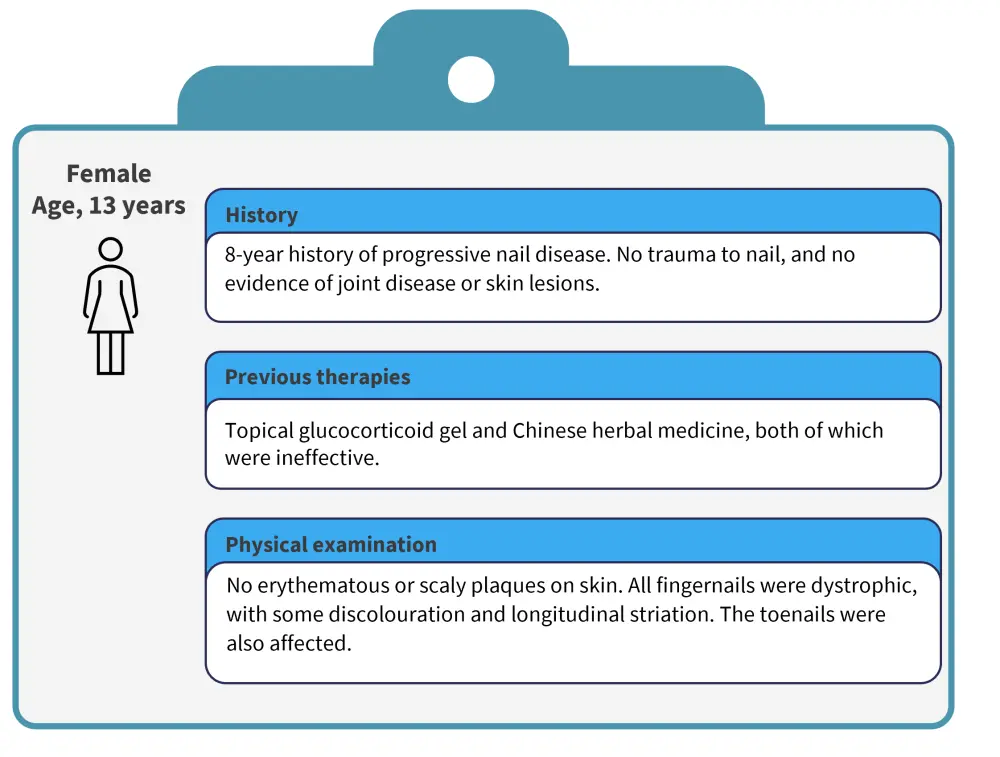
*Data from Wang, et al.1
The patient also underwent a longitudinal nail biopsy.1 The biopsy revealed hyperkeratosis, parakeratosis, and neutrophils in the nail plate. There were no infections identified in culture. The patient was screened for small molecule inhibitor treatment, and treatment with upadacitinib was started.1 Improvements in outcomes after treatment are shown in Figure 2.
Figure 2. Improvements in NAPSI and DLQI after treatment*
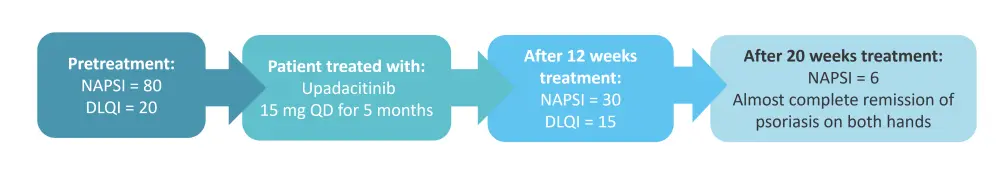
DLQI, Dermatology Life Quality Index; NAPSI, Nail Psoriasis Severity Index; QD, once daily.
*Data from Wang, et al.1
At Week 20, there was pitting and discolouration on only one finger.1 The results were maintained up to the 24-week follow-up evaluation. Psoriasis on the toenails also resolved with upadacitinib treatment. There were no adverse events during treatment.1
Conclusion
In this case study, treatment with upadacitinib led to improvements in Nail Psoriasis Severity Index and Dermatology Life Quality Index over 24 weeks, with no safety concerns.1 This suggests that upadacitinib may be an effective treatment option for patients with nail psoriasis; however, clinical trials are warranted. Upadacitinib is currently only approved in psoriatic arthritis for adult patients in the United States2 and Europe.3
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with plaque psoriasis do you see per month?

